HIV Medication & Statin Interaction Checker
Check Your Medication Combination
Safety Results
Enter your HIV medication and statin to see if they're safe together.
People living with HIV are living longer than ever. Thanks to modern antiretroviral therapy (ART), many are now managing HIV like a chronic condition - but that means dealing with new health challenges, like heart disease. Statins, the go-to drugs for lowering cholesterol and reducing heart attack risk, are often needed. But mixing them with HIV meds isn’t as simple as popping two pills. Some combinations can cause dangerous muscle damage, even life-threatening rhabdomyolysis. Knowing which statins are safe - and which are outright dangerous - isn’t optional. It’s essential.
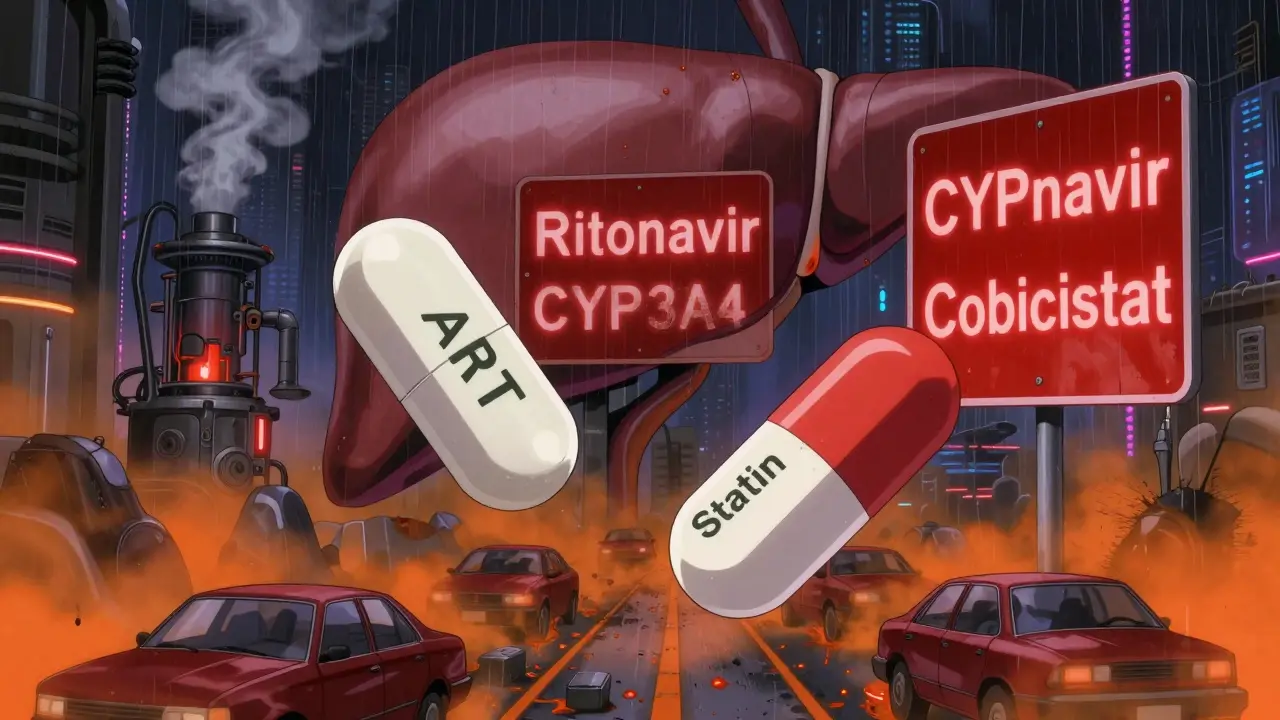
Why HIV Meds and Statins Don’t Always Get Along
The problem starts in your liver. Most statins are broken down by enzymes called CYP3A4 and transported by proteins like OATP1B1. Many HIV medications, especially those boosted with cobicistat or ritonavir, shut these enzymes down hard. When that happens, statins build up in your blood - sometimes to levels 20 times higher than normal. That’s not just a little extra cholesterol lowering. That’s a red flag for muscle breakdown. Think of it like traffic. CYP3A4 is a highway. Ritonavir and cobicistat are roadblocks. Statins are cars trying to get through. When the roadblocks are up, cars pile up. Too many cars = muscle damage. The FDA first warned about this in 2014, and updated those warnings as recently as 2023. The risk isn’t theoretical. Real people have ended up in the hospital with muscle pain, dark urine, and kidney failure because of these interactions.Statins You Must Avoid Completely
There are two statins that should never be taken with any HIV protease inhibitor or booster: simvastatin (Zocor) and lovastatin (Mevacor). That’s not a suggestion. It’s a hard contraindication. Why? Because they’re the most vulnerable. Studies show that when these two are mixed with drugs like darunavir/cobicistat, their blood levels can jump by up to 20-fold. The New York State Department of Health’s 2025 guidelines say it plainly: “Concomitant use is contraindicated.” The University of Liverpool’s HIV Drug Interactions database, updated monthly and used by clinicians worldwide, lists this combination as “severe risk.” There’s no safe dose. No exception. If you’re on a regimen like Prezcobix (darunavir/cobicistat), Symtuza, or even older combos like Kaletra (lopinavir/ritonavir), simvastatin and lovastatin are off the table. Period.Safe Statin Options - And How to Use Them
Good news: you don’t have to give up statins. Several options are safe - if you follow the rules. Pitavastatin (Livalo) is often the top pick. It’s mostly cleared by a different liver pathway (glucuronidation), so it doesn’t rely heavily on CYP3A4. That means fewer interactions. Studies show it works well with most ART, including boosted regimens, without needing dose cuts. It’s not available everywhere, but when it is, it’s a smart first choice. Pravastatin (Pravachol) is another solid option. Like pitavastatin, it’s handled by different enzymes. It’s older, cheaper, and well-studied in HIV populations. No dose adjustments needed for most HIV meds. It’s not as potent as newer statins, but for many people, it’s enough. Fluvastatin (Lescol) is metabolized by CYP2C9, so it avoids the main CYP3A4 trap. But here’s the catch: ritonavir can still slightly raise its levels (about 2-fold). So use it with caution, especially if you’re older or have kidney issues. It’s a backup, not a first-line. Atorvastatin (Lipitor) and rosuvastatin (Crestor) are powerful - and they can work - but only if you stick to low doses. For atorvastatin: if you’re on darunavir/cobicistat, don’t go over 20 mg per day. The US label says 20 mg. Some guidelines say 40 mg, but the safer path is 20 mg. If you’re on an unboosted INSTI like dolutegravir or bictegravir, you can use standard doses - up to 80 mg if needed. For rosuvastatin: maximum 10 mg per day if you’re on ritonavir or cobicistat. Never exceed that. Even at 10 mg, it’s still strong enough for most people with HIV and high cholesterol.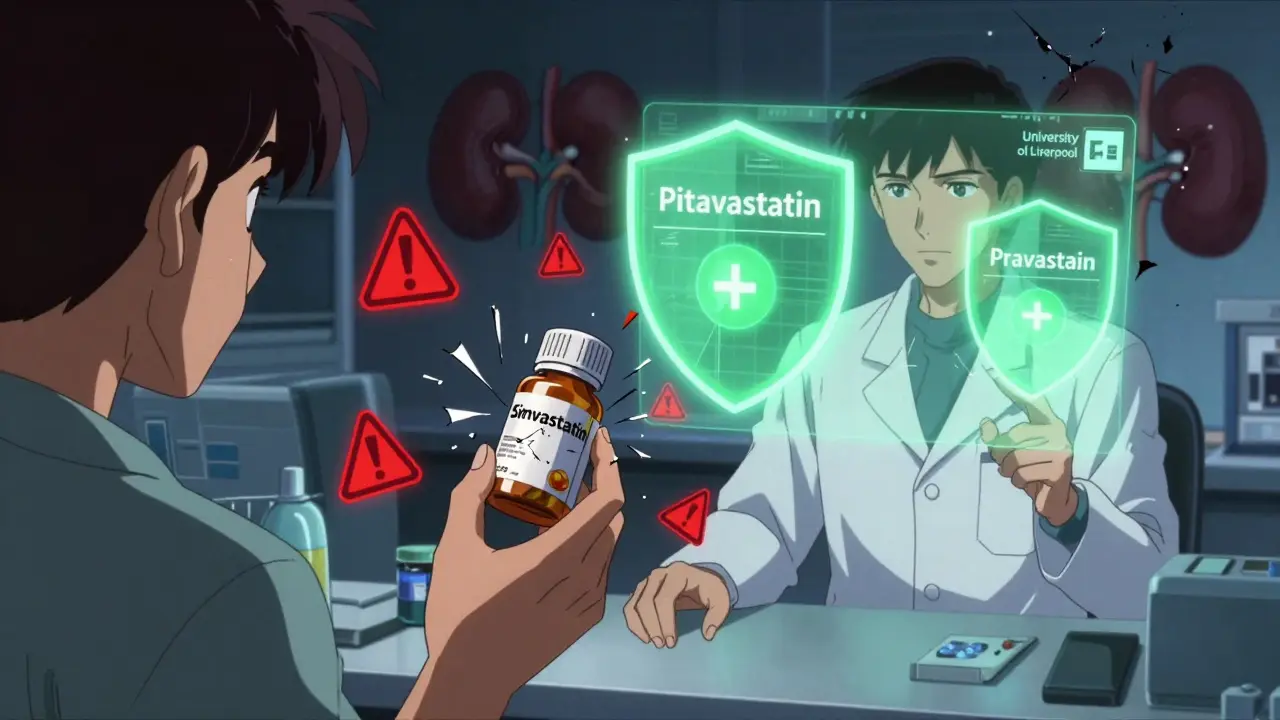
What About Newer HIV Drugs?
The good news is that newer HIV medications are much friendlier. Drugs like dolutegravir (Tivicay), bictegravir (in Biktarvy), and raltegravir (Isentress) don’t interfere much with CYP3A4. That means if you’re on one of these, you can usually take statins at normal doses - no dose cuts needed. That’s why many doctors now prefer INSTI-based regimens for patients who need statins. It’s not just about controlling HIV. It’s about making long-term heart health easier.Other Medications That Make Things Worse
It’s not just HIV meds. Other common prescriptions can pile on the risk. Some blood pressure pills - like felodipine and amlodipine - are also broken down by CYP3A4. If you’re on one of those plus a statin and a boosted HIV drug, you’re stacking the deck. Talk to your doctor about switching to a calcium channel blocker that doesn’t interact, like diltiazem or verapamil (though even those need checking). Don’t forget over-the-counter stuff. Gemfibrozil (Lopid), sometimes used for high triglycerides, is a big no-no with statins. It increases muscle toxicity risk. Better options? Fenofibrate or omega-3 fatty acids. They’re safer and just as effective.How to Stay Safe - Monitoring and Red Flags
Even with the right statin and dose, you need to watch for trouble. Muscle pain, weakness, or cramps - especially in your thighs or shoulders - are early signs. Dark, tea-colored urine means your muscles are breaking down and your kidneys are under stress. That’s a medical emergency. Your doctor should check your creatine kinase (CK) levels before you start a statin and then every 3-6 months if you’re on a boosted HIV regimen. Liver enzymes (ALT, AST) should also be monitored. If you’re over 65, have kidney disease, or take other interacting drugs, you need even closer watch. Don’t ignore symptoms. A little soreness after a workout is normal. Constant, unexplained pain? Not normal. Call your doctor.
What You Should Do Right Now
If you’re on HIV meds and taking a statin - or thinking about it - here’s your action list:- Find out exactly which HIV drugs you’re taking. Write them down - including boosters like cobicistat or ritonavir.
- Check which statin you’re on. If it’s simvastatin or lovastatin, stop taking it and call your doctor immediately.
- If you’re on atorvastatin or rosuvastatin, confirm the dose. If you’re on a boosted regimen and taking more than 20 mg (atorvastatin) or 10 mg (rosuvastatin), you’re at risk.
- Ask your doctor if you’re on an INSTI like dolutegravir or bictegravir. If yes, your statin options open up.
- Use the University of Liverpool’s HIV Drug Interactions Checker (it’s free, updated monthly, and trusted worldwide).
- Tell your doctor about every other medication - even supplements, herbal products, or OTC painkillers.
Why This Still Isn’t Common Knowledge
Despite clear guidelines, many doctors still don’t check for these interactions. A 2023 survey found only 58% of primary care providers routinely use interaction checkers before prescribing statins to people with HIV. That’s alarming. Part of the problem is complexity. There are over 98,000 possible drug combinations in the Liverpool database. No one can memorize them all. That’s why tools like the checker exist - and why you need to use them. The other part is complacency. Many assume statins are “safe” and HIV meds are “fine.” But when they mix, the danger is real. And the consequences? They’re not rare. They’re preventable.Bottom Line: You Can Have Both Heart Health and HIV Control
You don’t have to choose between managing your HIV and protecting your heart. But you do have to be smart about it. The right statin, at the right dose, with the right HIV regimen - that’s the formula. Pitavastatin and pravastatin are your safest bets. Atorvastatin and rosuvastatin can work - if you stick to the low doses. Simvastatin and lovastatin? Never. Your HIV doctor and your heart doctor need to talk. If they don’t, you need to make sure they do. Bring your pill bottle. Bring your list. Bring the Liverpool website. You’re not being difficult - you’re being responsible. Heart disease is the leading cause of death in people with HIV. Statins save lives. But only if they’re used safely. Know your meds. Know your risks. Ask the questions. Your muscles - and your future - depend on it.Can I take simvastatin with my HIV meds?
No. Simvastatin is absolutely contraindicated with all HIV protease inhibitors and pharmacokinetic boosters like cobicistat or ritonavir. Even low doses can cause life-threatening muscle damage. If you’re on any of these HIV drugs, switch to a safer statin like pitavastatin, pravastatin, or a low-dose atorvastatin or rosuvastatin.
Is atorvastatin safe with darunavir/cobicistat?
Yes, but only at a maximum of 20 mg per day. Higher doses can cause dangerous increases in statin levels. The US product label for Symtuza and Prezcobix specifically limits atorvastatin to 20 mg daily when used with cobicistat. Always start low and increase only under medical supervision.
What’s the safest statin for someone on HIV treatment?
Pitavastatin is generally the safest choice because it’s metabolized through a different liver pathway and has minimal interaction with HIV drugs. Pravastatin is also very safe and widely available. Both can usually be used without dose changes, even with boosted HIV regimens.
Can I take rosuvastatin with lopinavir/ritonavir?
Yes, but only at a dose of 10 mg per day or less. Lopinavir/ritonavir can increase rosuvastatin levels by up to three times. Higher doses raise the risk of muscle damage. Always confirm your dose with your doctor and get regular muscle and liver tests.
Do I need to stop statins if I switch HIV meds?
Not necessarily - but you must check again. Switching from a boosted regimen (like darunavir/cobicistat) to an unboosted INSTI (like bictegravir) may allow you to increase your statin dose. Conversely, switching to a boosted drug may require you to lower it. Always review your statin dose with your doctor after any HIV regimen change.
What should I do if I feel muscle pain while on statins and HIV meds?
Don’t ignore it. Muscle pain, weakness, or dark urine are signs of possible rhabdomyolysis - a medical emergency. Stop taking the statin and contact your doctor immediately. They may check your creatine kinase (CK) levels and liver enzymes. Never restart the statin without medical advice.
Can I use over-the-counter supplements with my HIV meds and statins?
Many supplements can interact. St. John’s Wort, for example, can lower HIV drug levels. Garlic supplements and grapefruit juice can raise statin levels. Always tell your doctor about every supplement, herb, or vitamin you take - even if you think it’s harmless. What seems natural can still be dangerous.
How often should I get blood tests if I’m on both HIV meds and statins?
Before starting a statin, get a baseline creatine kinase (CK) and liver function test. After starting, get tested every 3-6 months if you’re on a boosted HIV regimen. If you’re on an unboosted INSTI, annual testing may be enough. But if you develop muscle pain, get tested immediately - don’t wait.
Andrew Freeman
January 14, 2026 AT 14:38my uncle took simvastatin for 3 years and never had a heart issue
he died of cancer instead lol
Susie Deer
January 15, 2026 AT 11:02TooAfraid ToSay
January 15, 2026 AT 18:18they give you one pill then another then another
then you wake up one day with no muscles and a kidney that looks like a raisin
they call it science i call it a death sentence with a prescription pad
Allison Deming
January 17, 2026 AT 08:29Vicky Zhang
January 19, 2026 AT 06:10you’re not alone
so many people are scared to even ask their doctor about this stuff
but you read the article, you’re thinking about your health, you’re trying to do right
that’s huge
and if you’re on pitavastatin or pravastatin? you’re already winning
you’re not just surviving-you’re thriving
Dylan Livingston
January 19, 2026 AT 23:14statins and HIV meds interact
next you’ll tell me water is wet and the sky is blue
and yet here we are, 2025, and people still need a 2000-word essay to understand that mixing drugs without checking isn’t genius
it’s just tragic
says haze
January 21, 2026 AT 23:13Anna Hunger
January 23, 2026 AT 10:05Sarah Triphahn
January 25, 2026 AT 06:10but you know what’s really dangerous?
people who don’t take them
heart disease kills more people with HIV than the virus itself
if you’re scared of side effects, you’re scared of living
Alvin Bregman
January 26, 2026 AT 20:30never looked up anything
but now i feel kinda dumb
maybe i should check my pills
thanks for the nudge
Sarah -Jane Vincent
January 27, 2026 AT 17:11the government and big pharma are hiding the truth
statins don’t lower cholesterol
they’re just a cover-up for the real cause of heart disease: 5G radiation and chemtrails
and cobicistat? it’s not a booster-it’s a mind-control agent
you think you’re safe with pitavastatin?
you’re just being programmed to believe the lie