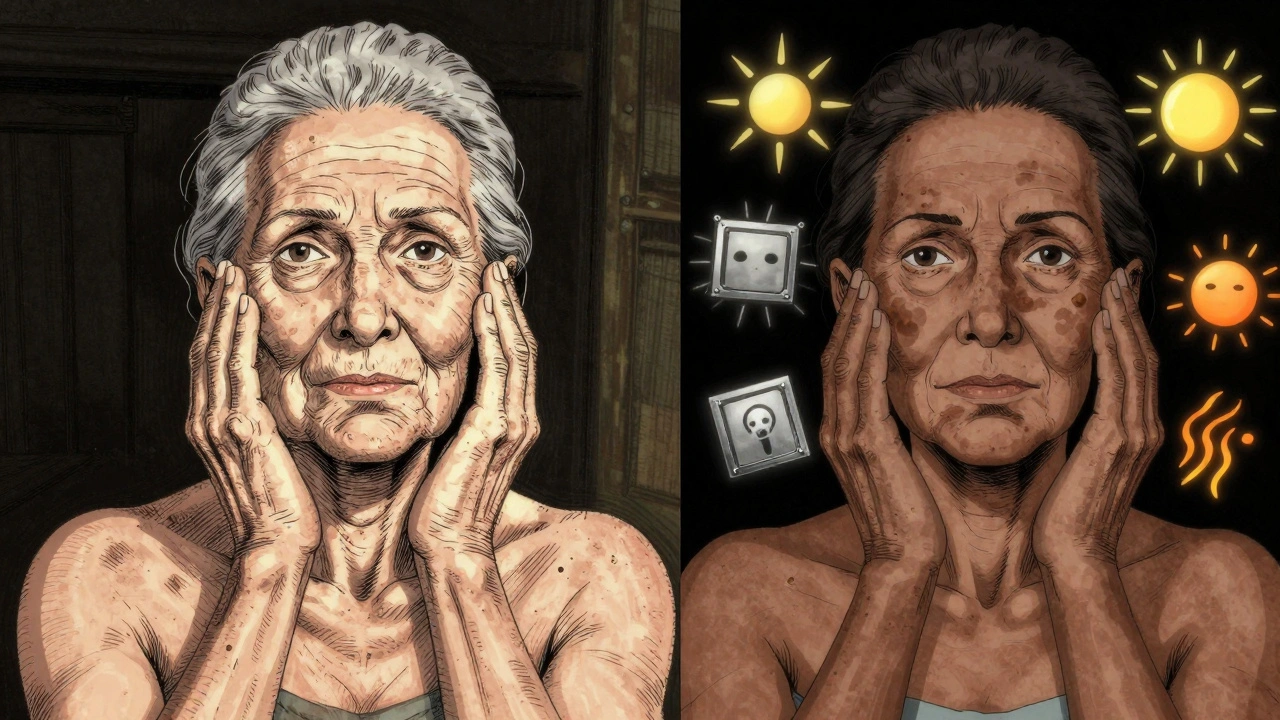
Dark spots on your face don’t always mean the same thing. Two of the most common causes-melasma and sun damage-look similar but behave completely differently. One is triggered by hormones and light, the other by years of sun exposure. Treat one the same way as the other, and you could make it worse. If you’ve tried creams, lasers, or sunscreens without lasting results, you’re not alone. Most people don’t realize they’re treating the wrong problem.
What’s Really Causing Your Dark Patches?
Melasma shows up as large, blurry patches on the cheeks, forehead, or upper lip. It’s not just a sun spot. It’s a reaction to hormones, heat, and visible light-not just UV. Up to 90% of cases occur in women, especially during pregnancy, while on birth control, or after menopause. People with medium to dark skin tones (Fitzpatrick III-VI) are 3 to 5 times more likely to develop it. That’s why it’s so common in Black, Asian, and Hispanic populations.
Sun damage, or solar lentigines, looks different. These are small, crisp, brown spots on the nose, hands, shoulders, or chest. They show up slowly over time. By age 60, about 90% of fair-skinned people have them. They’re caused by direct UV exposure damaging melanocytes-the cells that make pigment. Unlike melasma, they don’t respond to hormones. They’re purely a result of accumulated sun exposure.
Here’s the key difference: melasma is a chronic condition. Sun damage is a visible sign of past harm. One can be managed. The other can be reversed.
Why Most Sunscreens Don’t Work for Melasma
You’ve probably been told to wear SPF 30 or higher. That’s good advice-for sunburn and skin cancer. But for melasma? It’s not enough.
Visible light (the blue and green wavelengths you see) and infrared heat can trigger melasma just as much as UV rays. Regular sunscreens block UV but let most visible light through. That’s why many people with melasma still get worse-even with sunscreen.
Studies show visible light contributes to 25-30% of melasma cases. The solution? Mineral sunscreens with iron oxides. Zinc oxide and titanium dioxide block UV, but iron oxides block visible light. Look for tinted sunscreens labeled “broad-spectrum with iron oxide.” They’re not just for cosmetics-they’re medical-grade protection.
And don’t forget: UV and visible light come through windows. If you sit near a window at home or in your car, you’re still exposed. Daily SPF 50+ with iron oxide isn’t optional-it’s the foundation of every successful melasma treatment.
Topical Treatments: What Actually Works
Not all creams are created equal. Here’s what dermatologists use for each condition:
- Hydroquinone (4%): The gold standard for melasma. It blocks the enzyme that makes melanin. Used alone, it helps about 30% of people. But when combined with tretinoin and a corticosteroid (a triple combo), improvement jumps to 50-70% in 12 weeks. Limit use to 3 months at a time-longer increases the risk of ochronosis, a rare but permanent darkening.
- Tretinoin (0.025-0.1%): This retinoid speeds up skin cell turnover. It doesn’t lighten pigment directly, but it helps flush it out. Use it every other night to avoid irritation. Start low-your skin needs time to adjust.
- Vitamin C (10-20% L-ascorbic acid): A powerful antioxidant. It reduces existing melanin and stops new pigment from forming. Use it in the morning under sunscreen. It also helps protect against pollution and blue light.
- Tranexamic acid (5%): An emerging option. Originally a blood thinner, it’s now used topically to block signals that trigger melanin production. Studies show 45% improvement in melasma after 12 weeks with no major side effects.
- Kojic acid, niacinamide, azelaic acid: Good alternatives if you can’t use hydroquinone. Niacinamide (5%) reduces pigment transfer to skin cells. Azelaic acid (15-20%) works well for both melasma and post-inflammatory spots.
For sun damage? Hydroquinone helps, but it’s not the best. Lasers work faster and more predictably.
Laser and Light Therapies: When to Use Them
IPL (Intense Pulsed Light) is great for sun spots. It targets brown pigment with light energy. The spots darken, then flake off in 3-5 days. Most people need 1-2 sessions. Results last years-if you keep wearing sunscreen.
But IPL is dangerous for melasma. Heat from the light can trigger more pigment. Up to 40% of melasma patients get worse after IPL. Dermatologists won’t even consider it until the skin has been suppressed with topical treatment for 8-12 weeks. That’s called a “melanocyte rest.”
For melasma, safer options include low-energy Q-switched lasers, fractional non-ablative lasers, or chemical peels (like glycolic or lactic acid). But even these require caution. Darker skin types (Fitzpatrick IV-VI) have a higher risk of post-inflammatory hyperpigmentation from any procedure. That’s why 40% of hyperpigmentation cases are in these skin tones-and why treatment must be personalized.
Why Melasma Comes Back-Even After Success
If your melasma improved but returned after a few months, you’re not failing. You’re normal.
Studies show over 80% of melasma patients relapse within a year if they stop treatment. That’s because the triggers-hormones, light, heat-are always there. Melasma isn’t cured. It’s managed.
Think of it like high blood pressure. You don’t stop taking the pill just because your numbers are normal. Same here. Maintenance is non-negotiable.
Successful long-term control means:
- Daily SPF 50+ with iron oxide (even indoors)
- Evening use of tretinoin or tranexamic acid
- Occasional chemical peels every 3-6 months
- Avoiding heat: hot yoga, saunas, steam rooms
- Replacing hormonal birth control if possible
And here’s the hard truth: 65% of patients don’t use their prescriptions consistently. They skip days. They use too little sunscreen. They think “I’m indoors, so I’m safe.” That’s why most treatments fail-not because they don’t work, but because they’re not used right.
What Not to Do
Here are the biggest mistakes people make:
- Using hydroquinone for more than 3 months straight-risk of ochronosis increases.
- Starting lasers without pre-treating melasma first-can make it worse.
- Using chemical peels on dark skin without a dermatologist-high risk of PIH.
- Believing OTC creams (like “brightening” serums) will fix melasma-they rarely do.
- Skipping sunscreen on cloudy days-up to 80% of UV penetrates clouds.
And don’t assume all dark spots are the same. Post-inflammatory hyperpigmentation (PIH) from acne or eczema looks similar but appears where there was inflammation-not necessarily sun-exposed areas. It responds poorly to lasers and needs different topicals like azelaic acid or niacinamide.
The Future of Treatment
Research is moving fast. Cysteamine cream (10%) showed 60% improvement in melasma with minimal irritation in recent trials. Tranexamic acid pills are now being studied for severe cases. Some dermatologists are testing genetic tests to predict who responds best to which treatment.
But the biggest breakthrough isn’t a new cream-it’s awareness. More people now know that sunscreen isn’t optional for melasma. More dermatologists are prescribing triple combos upfront. More patients are learning that consistency beats quick fixes.
The global market for hyperpigmentation treatments is growing fast-$12.7 billion in 2022 and climbing. But money doesn’t fix this. Knowledge does.
What to Do Today
If you’re dealing with dark spots:
- Take a photo of your spots. Note where they are and when they appeared.
- Check if they’re symmetrical (melasma) or scattered (sun damage).
- Start using a mineral sunscreen with iron oxide every morning. Use a quarter teaspoon for your face.
- Stop using harsh scrubs or DIY remedies. They irritate and worsen pigmentation.
- See a dermatologist. Don’t wait. The sooner you get the right diagnosis, the sooner you’ll see results.
There’s no magic bullet. But with the right approach, melasma can fade. Sun damage can vanish. And you don’t need to spend hundreds a month to make progress. Just be consistent. Be patient. And protect your skin like your life depends on it-because for your skin, it does.
Is melasma the same as sun spots?
No. Melasma is hormone-driven and appears as large, blurry patches on the face, often triggered by sunlight, heat, and visible light. Sun spots (solar lentigines) are small, well-defined brown spots caused by long-term UV exposure and appear on sun-exposed areas like hands and shoulders. They respond differently to treatment-melasma can worsen with lasers, while sun spots improve.
Can I treat melasma with over-the-counter products?
Most OTC brightening creams won’t fix melasma. Ingredients like niacinamide or kojic acid may help slightly, but they’re not strong enough for significant improvement. Prescription topicals like hydroquinone, tretinoin, and tranexamic acid are needed for real results. Over-the-counter products are often a delay tactic-many patients spend months on them before seeing a dermatologist.
Do I need to wear sunscreen indoors?
Yes, especially for melasma. Visible light and infrared radiation pass through windows and can trigger pigment production. Even sitting near a sunny window can worsen melasma. Daily use of a mineral sunscreen with iron oxide is essential-even on cloudy days or when you’re inside.
Why does my melasma get worse in summer?
Summer means more UV, visible light, and heat-all three trigger melasma. Heat increases blood flow to the skin, which activates melanocytes. UV and visible light directly stimulate pigment production. That’s why melasma often flares during summer and improves in winter. Strict sun protection is even more critical during these months.
Can laser treatments cure melasma?
No. Lasers can improve melasma, but they don’t cure it. Heat from lasers can trigger more pigment if used too early or too aggressively. Dermatologists only use lasers after 8-12 weeks of topical treatment to suppress melanocyte activity. Even then, recurrence rates are high without ongoing maintenance. Melasma requires lifelong management, not a one-time fix.
How long does it take to see results from topical treatments?
It takes 8-12 weeks to see noticeable improvement with topical treatments like hydroquinone and tretinoin. Some people see changes after 4 weeks, but full results take 3-6 months. Patience is key. Stopping early because you don’t see immediate results is the most common reason treatment fails.
Is hydroquinone safe to use long-term?
Hydroquinone is safe for short-term use (up to 3 months) under medical supervision. Long-term use without breaks increases the risk of ochronosis-a rare condition where the skin turns blue-black. Most dermatologists recommend cycling: 3 months on, 1-2 months off. Alternatives like tranexamic acid or azelaic acid can be used during breaks.
Can men get melasma?
Yes, but it’s rare. Only about 10% of melasma cases occur in men. When it does, it’s often linked to hormonal changes, certain medications, or intense sun exposure. Men are more likely to have sun damage than melasma, so proper diagnosis is essential before starting treatment.

Michael Dioso
December 6, 2025 AT 01:20Wow, another article telling me I’ve been doing everything wrong for years. Guess what? I’ve been using SPF 50 since 2018 and I still look like a raccoon after a nap in a tanning bed. Iron oxide? Who even makes that stuff? I thought sunscreen was supposed to be white and sticky, not some fancy tinted foundation for people who think they’re in a Kardashian ad.
sean whitfield
December 7, 2025 AT 11:21They don’t want you to know the truth. Sunscreen doesn’t block visible light because the FDA and Big Pharma are in bed with the makeup industry. Iron oxide? That’s just pigment to make you think you’re protected. Real protection is staying inside. Or better yet-stop having hormones. That’s the real root cause. Melasma is just your body screaming for a revolution.
Jennifer Patrician
December 9, 2025 AT 01:57Oh please. You think a tinted sunscreen is going to save you? I used hydroquinone for 3 months and my face turned into a bruise. Then I found out my dermatologist was using my skin as a test lab for some new drug trial. You think you’re being careful? You’re just another lab rat with a $40 bottle of vitamin C. And don’t even get me started on ‘maintenance’-that’s just a fancy word for ‘you’ll never be free.’
Mark Curry
December 10, 2025 AT 20:28It’s weird how we treat skin like it’s a problem to be solved instead of a reflection of our whole life. Stress, sleep, diet, hormones, sun, windows, even the air we breathe-it’s all connected. Maybe the real fix isn’t a cream or a laser, but learning to slow down. I’ve been using niacinamide for 6 months. Not because it’s magic, but because it’s gentle. And sometimes, gentle is enough.
Manish Shankar
December 12, 2025 AT 00:57Respected author, your detailed analysis is profoundly insightful. I am from India, and melasma is extremely common here due to high UV index and hormonal factors. Many patients delay consultation due to cultural stigma and reliance on over-the-counter creams. Your emphasis on medical-grade sunscreen with iron oxide is critical. I have advised my patients to use tinted mineral sunscreens daily, and outcomes have improved significantly when compliance is maintained.
Lynette Myles
December 12, 2025 AT 03:29Annie Grajewski
December 12, 2025 AT 04:05so i tried the triple combo and my skin looked like a zombie for 3 weeks. like, i couldnt leave the house. but then-POOF. it started fading. now i use tranexamic acid and act like i dont care. also, i wear my sunscreen like a second skin. even when i’m crying in my car at 2am. because my face is worth it. also, dont trust your auntie’s turmeric mask. it’s not helping. it’s just sticky.
Jimmy Jude
December 13, 2025 AT 01:38Let me tell you something about melasma. It’s not just skin. It’s trauma. It’s the 3 a.m. panic when you look in the mirror and realize your face is changing faster than your life. It’s the years of being told ‘just wear sunscreen’ like that’s a cure. It’s the shame of hiding behind makeup that still doesn’t cover it. And yeah, maybe you’re right-maybe it’s not curable. But you know what? I’m not giving up. I’m not hiding. I’m not letting some dermatologist tell me I’m not trying hard enough. I’m not a problem to be fixed. I’m a person who’s still standing. And my skin? It’s just part of the story.