Every year, the FDA approves hundreds of generic drugs - and each approval saves the U.S. healthcare system billions. But the numbers don’t stay the same. Some years, the savings spike. Others, they drop. Why? It’s not random. It’s tied to which drugs lose their patents and when.
What Exactly Are These Savings?
When a brand-name drug’s patent expires, generic versions enter the market. Prices usually plunge - often by more than 70%. The savings come from two places: patients pay less out of pocket, and insurers pay less overall. But not all savings are counted the same way. The FDA measures savings from new generic approvals - meaning drugs that were brand-only until that year. They track sales for 12 months after approval and calculate the difference between what people would’ve paid for the brand versus what they actually paid for the generic. This is called the first-generic savings. Separately, the Association for Accessible Medicines (AAM) counts all generic drug savings in a year - including every generic already on the market. This number is much bigger because it includes decades of generic use, not just new entries.Year-by-Year Breakdown: First Generic Approvals (FDA Data)
If you’re looking at the impact of new generic entries, here’s what happened over the last few years:- 2018: $2.7 billion saved from 36 first-time generic approvals
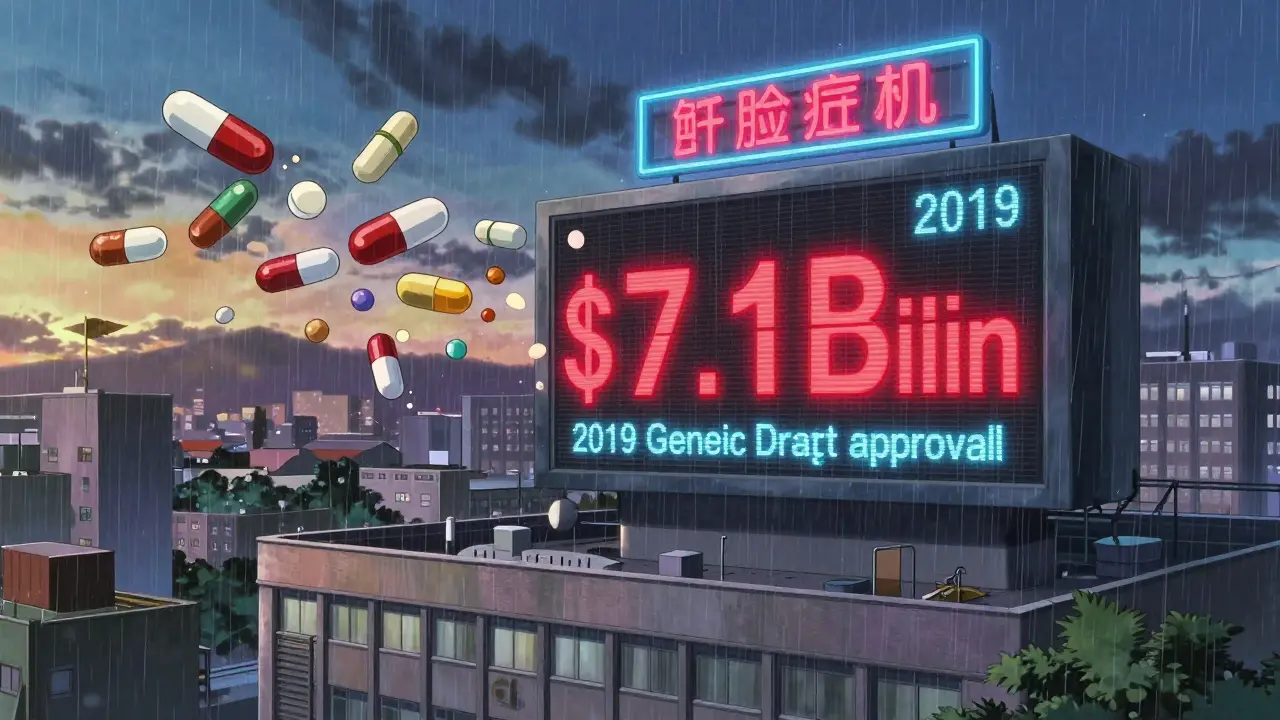
- 2019: $7.1 billion saved - the highest year on record. This was driven by a handful of blockbuster drugs losing patent protection, including a major cholesterol med that alone saved $1.5 billion in its first year.
- 2020: $1.1 billion saved. A quiet year. No major drug patents expired.
- 2021: $1.37 billion saved. Five drugs accounted for half of this total. One cancer treatment, in particular, drove $750 million in savings.
- 2022: $5.2 billion saved. A huge jump. Why? Several high-volume drugs hit the market, including a widely used diabetes medication and a common blood pressure pill.
Notice the pattern? Savings aren’t steady. They’re lumpy. One big patent cliff can double the year’s savings. The next year, if no major drugs expire, the number drops again. That’s why looking at a single year can be misleading.
Total Generic Savings: The Bigger Picture (AAM Data)
Now, step back. Look at the full picture - every generic drug used in a year, not just the new ones.- 2020: $338 billion saved
- 2022: $408 billion saved
- 2023: $445 billion saved
This is the real story. In 2023 alone, generics saved Americans more than $445 billion. That’s more than the entire annual budget of the U.S. Department of Education. And 90% of all prescriptions filled in the U.S. are now generics.
Breakdown by payer:
- Medicare: $137 billion saved ($2,672 per beneficiary)
- Commercial insurers: $206 billion saved
- Medicaid: $102 billion saved
By therapy area:
- Heart disease: $118.1 billion saved
- Mental health: $76.4 billion saved
- Cancer: $25.5 billion saved
That’s not just numbers. That’s people. A diabetic paying $30 a month instead of $300. A cancer patient on a generic that cuts their out-of-pocket cost from $1,200 to $80. That’s what this data means.
How Are Savings Calculated?
The FDA’s method is precise. They take the brand-name price at the time of generic approval and compare it to the generic price 12 months later. Then they multiply by how many pills were sold. They also account for the fact that brand-name prices often drop after a generic enters - sometimes by 50% or more - because manufacturers know they can’t compete. The formula looks like this:Savings = (Brand price − Generic price) × Generic volume + (Brand price reduction × Brand volume)
AAM takes a broader view. They estimate what total spending would’ve been if no generics existed - then subtract what was actually spent. It’s a backward-looking calculation, but it shows the real, cumulative impact.
Who Benefits the Most?
It’s not just insurers. Patients pay less too. In 2019, the average generic copay was $6.97. About 92% of generic prescriptions cost $20 or less. For chronic conditions like high blood pressure or asthma, that means $20 a month instead of $300. But here’s the catch: not all savings reach patients. Pharmacy benefit managers (PBMs) negotiate rebates with drugmakers. Often, those rebates go to insurers or employers - not the person at the pharmacy counter. A 2023 Senate investigation found only 50-70% of generic savings actually lower patient costs. State programs see it clearly. California’s Medi-Cal saved $23.4 billion in 2023. Alaska saved $354 million. Population size matters. Bigger states get bigger savings.Why Do Some Years Have More Savings?
It comes down to patents. The biggest savings happen when a blockbuster drug loses exclusivity. In 2019, a single cholesterol drug called Repatha went generic and saved $1.5 billion in its first year. In 2022, two diabetes drugs - Januvia and Tradjenta - hit the market as generics and together saved over $2 billion. The FDA approved 742 generic applications in 2022 - the most in a decade. But only 16 of those were first-time generics. The rest were additional versions of drugs that already had generics. Those add competition, but don’t create massive savings like a first generic does.
What’s Changing Now?
More complex drugs are coming off patent. Biologics - like insulin and rheumatoid arthritis drugs - are harder to copy. That’s why biosimilars (generic versions of biologics) are growing. As of August 2024, the FDA had approved 59 biosimilars. They’re not saving as much yet - but they will. The FDA is also speeding things up. Thanks to the Generic Drug User Fee Amendments (GDUFA), 95% of generic applications are reviewed in 10 months or less. That means faster market entry, and faster savings. But challenges remain. Brand companies use legal tricks - like patent extensions and REMS (Risk Evaluation and Mitigation Strategies) - to delay generics. Some lawsuits can push back generic entry by years.What’s Next?
By 2033, U.S. generic drug revenue is projected to hit $131.8 billion. That’s because more blockbusters are expiring: drugs for Alzheimer’s, heart failure, and obesity are all on the horizon. The AAM estimates total generic and biosimilar savings will reach $3.9 trillion between 2014 and 2028. That means annual savings could hit $500 billion by the end of this decade. The key takeaway? Generic drugs aren’t just cheaper. They’re essential. They keep millions of Americans on their meds. They keep healthcare spending from exploding. And every year, the savings depend on one thing: which patents expire.Why do generic drug savings vary so much from year to year?
Savings jump when a high-revenue brand-name drug loses its patent and a generic enters. If no major drugs expire in a given year, savings drop. For example, 2019 had $7.1 billion in savings because several expensive drugs went generic. 2020 had only $1.1 billion because few patents expired. It’s not about how many generics are approved - it’s about how expensive the drugs are.
Do patients always save money when a generic is approved?
Not always. While generics are cheaper for pharmacies and insurers, savings don’t always reach patients. Pharmacy benefit managers (PBMs) often keep rebates from drugmakers, so even if a drug’s price drops, your copay might not change. Studies show only 50-70% of generic savings are passed on to consumers. Medicaid and Medicare programs see the biggest savings, but out-of-pocket costs for patients can still be high if their plan doesn’t adjust.
How does the FDA decide which generics to approve?
The FDA doesn’t choose which drugs to approve - manufacturers apply for approval after a brand-name drug’s patent expires. The FDA reviews each application to make sure the generic is bioequivalent: it works the same way, in the same amount of time, with the same safety profile. The agency reviews about 1,000 applications each year. Speed matters: under GDUFA, 95% are reviewed within 10 months.
Are biosimilars as effective as traditional generics?
Biosimilars are not exact copies like traditional generics - they’re highly similar versions of complex biologic drugs, like insulin or cancer treatments. They’re not identical because biologics are made from living cells, not chemicals. But the FDA requires them to show no clinically meaningful differences in safety or effectiveness. As of 2024, 59 biosimilars have been approved. They’re slower to adopt, but their savings are growing.
Can brand-name companies block generic entry?
Yes. Some use legal tactics to delay generics - like filing lawsuits over minor patent changes, or using REMS programs (safety rules) to restrict generic access. The FDA’s 2023 Drug Competition Action Plan targets these practices. In 2022, the agency identified 20 cases where brand companies delayed generic entry by more than a year. These delays cost the system billions.
How do generic savings affect insurance premiums?
Lower drug costs help keep insurance premiums from rising too fast. In 2023, generics saved commercial insurers $206 billion. Without those savings, premiums for employer-sponsored plans could be 10-15% higher. Medicare and Medicaid also rely on generics to control spending. If generics disappeared, Medicare’s Part D program alone would cost over $200 billion more each year.
What’s the difference between a first generic and a follow-on generic?
A first generic is the very first generic version of a brand-name drug. It’s the one that breaks the monopoly and causes the biggest price drop. Follow-on generics come later - other companies make the same drug. They add competition, which keeps prices low, but don’t create big savings spikes. In 2022, 742 generic applications were approved, but only 16 were first generics. The rest were follow-ons.
Why do some generic drugs cost more than others?
It’s not about the drug - it’s about competition. If only one or two companies make a generic, prices stay higher. If five or more are competing, prices drop sharply. Some generics - like injectables or complex pills - are harder to make, so fewer companies enter the market. That’s why some generics cost $50 a month while others cost $5.
Is the FDA’s savings data reliable?
Yes. The FDA uses real sales data from manufacturers and pharmacies. They track prices and volumes for 12 months after each approval. Their methodology is transparent and peer-reviewed. Independent analysts at Drug Patent Watch and Statista confirm the numbers align with market trends. The data may be conservative - it doesn’t count long-term savings from reduced hospitalizations - but it’s accurate for what it measures.
What’s the future of generic drug savings?
Savings will keep growing, but the pace may slow. More complex drugs are coming off patent - like obesity and Alzheimer’s treatments - which will create new savings opportunities. Biosimilars will add billions more. But if brand companies continue delaying generics with legal tactics, savings could be held back. The next big wave depends on policy, competition, and whether regulators can keep the system open.
Elan Ricarte
February 8, 2026 AT 00:57Let me tell you something - this whole 'generic drug savings' thing is a goddamn miracle. I used to pay $400 a month for my dad's cholesterol med. Now? $12. That's not a number, that's a fucking lifeline. And yeah, 2019 was insane - $7.1 billion from one drug? That's like slapping Big Pharma in the face with a wad of cash they didn't expect to lose. But here's the kicker: most of that savings never makes it to the patient. PBMs are sucking the blood out of this system like vampires in a suit. We need to cut them out. Not regulate. Cut.
Camille Hall
February 9, 2026 AT 21:39Really appreciate this breakdown. It’s easy to think 'generics = cheap' and move on, but the real story is how they quietly hold up the whole healthcare system. I work in a community clinic - every day, someone thanks us because their insulin went from $500 to $30. That’s not policy talk. That’s someone eating, working, living. And yeah, the big patent cliffs matter, but it’s the steady drip of follow-on generics that keeps prices low long-term. We need to protect both.
Ritteka Goyal
February 11, 2026 AT 02:17Brooo this is why INDIA is the pharmacy of the world!! We make 40% of ALL generics globally and USA just sits there like a lazy king with a golden credit card. You guys pay 10x for same pill we make in Tamil Nadu for $0.10. Why? Because your pharma lobby owns Congress. I saw a guy in Mumbai with diabetes - he buys 30 pills for 15 rupees. You pay $300. I mean… seriously? This is colonialism with a stethoscope. FDA should just import directly from India and cut out the middlemen. Stop being so damn soft.
THANGAVEL PARASAKTHI
February 11, 2026 AT 13:05Yeah i agree with the india comment but also… its not that simple. We make the pills but we dont always get the money. The patents are US law. And yeah we have great manufacturing but the US still controls the supply chain. Also biosimilars? India is behind here. We need to invest more in R&D not just production. And dont forget - some generics are made in China now too. So its not just India vs USA. Its global. But yeah, the price gap is wild. My cousin in Hyderabad pays $2 for a blood pressure med that costs $120 here. Its not fair.
Chelsea Deflyss
February 12, 2026 AT 02:12Umm… so if generics save so much money, why are my premiums still going up? This whole post feels like a PR stunt. You say '90% of prescriptions are generics' but you don't mention that 70% of those are still under $20 copay - which means insurance companies are still milking us. Also, who approved that 'first-generic' math? Sounds like a fantasy spreadsheet. I’ve been on meds for 12 years. I’ve never seen a $1.5 billion savings in my wallet. This is just woke accounting.
Scott Conner
February 13, 2026 AT 20:41So if the FDA approves 742 generics in a year but only 16 are first-time, does that mean 97% of the 'savings' we're talking about are just from competition, not new entry? That’s wild. I always thought the big numbers came from new drugs going generic. But if it’s mostly follow-ons… then why do the big spikes happen? Maybe it’s not about quantity - it’s about which follow-ons are actually competitive. Like if five companies start making a diabetes drug, prices collapse. But if only two do? Not so much. Food for thought.
Sam Dickison
February 15, 2026 AT 20:18From a pharmacoeconomics standpoint, the FDA’s methodology is actually quite elegant - it isolates the marginal impact of first-entry generics, which is critical for policy modeling. The AAM aggregate data is useful for macroeconomic forecasting, but it obscures the causal mechanism. The real policy lever is incentivizing timely generic entry - not just volume. The patent cliff phenomenon is a textbook example of monopoly rent dissipation. We need to tighten REMS loopholes and enforce GDUFA timelines more aggressively. Otherwise, we’re just redistributing wealth from patients to PBMs and brand manufacturers via legal arbitrage.
Karianne Jackson
February 16, 2026 AT 00:42OMG I just cried reading this. My mom has lupus. She was paying $1,100 a month. Now? $75. That’s not a statistic. That’s her being able to go to her granddaughter’s recital. That’s her sleeping through the night. I don’t care if it’s $7.1 billion or $7.10 - if it saves one person, it’s worth it. I’m so tired of people talking about numbers and not people. This? This is why I fight. Thank you.
Tom Forwood
February 16, 2026 AT 08:57Hey, just wanted to say - as someone who grew up in rural Alabama, I didn’t even know generics existed until I was 25. My grandma took pills in a shoebox labeled 'blue for heart, white for pain.' No one explained it. So when I saw my first generic label - 'same as Lipitor, $6' - I thought I’d been scammed. Then I checked the bottle. Same pill. Same effect. That’s when I got it. This isn’t just economics. It’s education. We need to teach people how to read labels. And yeah - the big savings years? Those are the ones that change lives. Not the quiet ones.
Jacob den Hollander
February 16, 2026 AT 18:33Thank you for sharing this - really. I’ve been on a generic for anxiety for five years now. It’s saved me over $15,000. But what’s harder to measure? The peace of mind. Knowing I can afford to take it. Knowing I won’t have to choose between rent and refills. That’s the real savings. And when a drug like Januvia goes generic? It’s not just a price drop. It’s a whole community breathing easier. I’ve seen it. I’ve lived it. So yeah - the numbers matter. But the quiet moments? Those are the ones that keep us going.
Andrew Jackson
February 17, 2026 AT 00:30It is a profound moral failing of the American republic that we have allowed the pharmaceutical industry to extract such exorbitant rents from our citizens under the guise of 'innovation.' The Founding Fathers would be appalled. A nation that permits its people to die because they cannot afford a pill that costs pennies to produce is not a republic - it is a plutocracy draped in the trappings of democracy. The FDA’s approval of generics is not a benevolent act; it is a reluctant concession wrested from the jaws of corporate tyranny by the relentless pressure of public outrage. We must not be grateful for the crumbs - we must demand the entire table. And then we must burn it down.