Every year, millions of older adults reach for over-the-counter sleep aids or allergy pills containing diphenhydramine or doxylamine-brands like Benadryl or Unisom-thinking they’re harmless. But for people over 65, these common meds can trigger confusion, falls, and even accelerate memory loss. The truth? First-generation antihistamines aren’t just outdated-they’re dangerous for older bodies. And yet, they’re still widely used, often without anyone realizing the risk.
Why Elderly Bodies React Differently
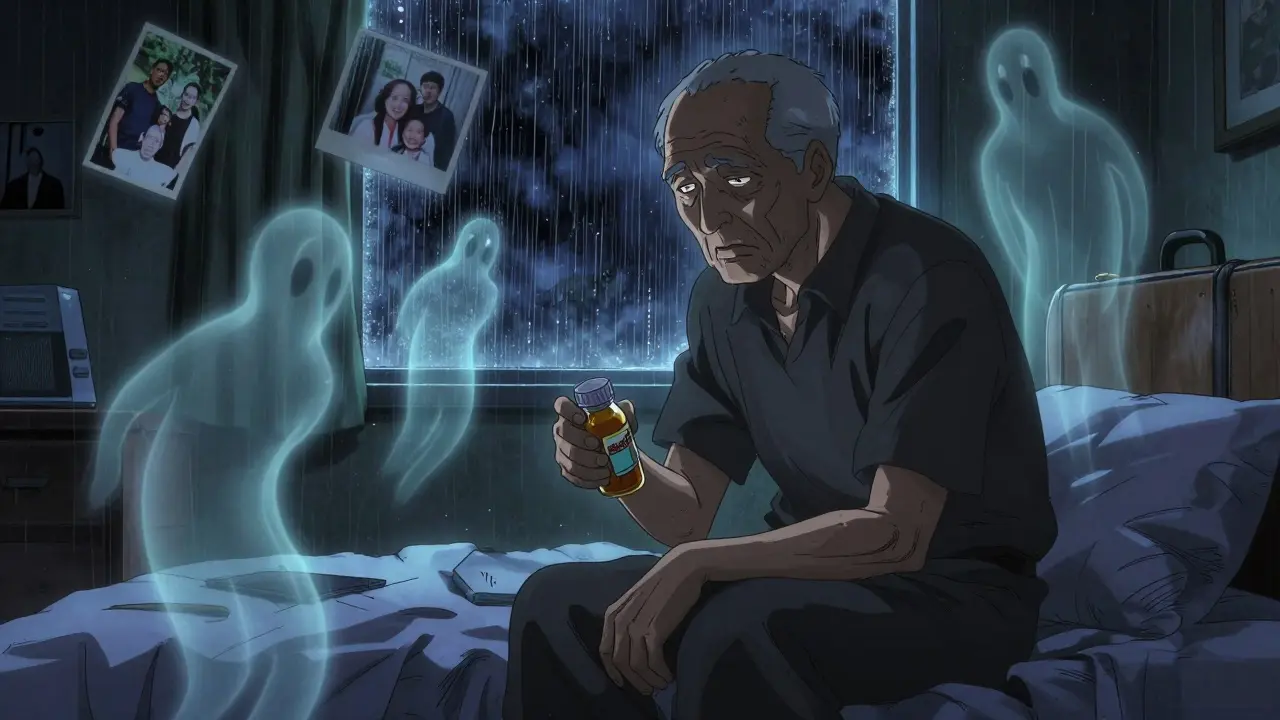
As we age, our bodies change in ways that make drugs behave unpredictably. The liver and kidneys don’t process medications as efficiently. Fat increases, muscle mass decreases, and the blood-brain barrier becomes more porous. For antihistamines, this means first-generation drugs like diphenhydramine, chlorpheniramine, and doxylamine slip easily into the brain, where they block acetylcholine-a key neurotransmitter for memory, focus, and muscle control. This isn’t just drowsiness. It’s a full-blown anticholinergic effect. The body’s natural supply of acetylcholine drops with age, so when these drugs block what’s left, the result is a double hit. Older adults don’t just feel sleepy-they get confused, disoriented, or even hallucinate. One caregiver in Hobart told me her 81-year-old husband started packing his bags at 2 a.m., convinced he needed to ‘go home,’ even though he’d lived in the same house for 50 years. He’d taken Benadryl for a stuffy nose. The confusion vanished within 48 hours after stopping it.The Real Danger: Falls and Fractures
Dizziness and drowsiness don’t just ruin sleep-they ruin safety. A 2018 meta-analysis of five major studies found that elderly people taking first-generation antihistamines had more than double the risk of serious falls or fractures compared to those who didn’t. The odds ratio? 2.03. That’s not a small bump. That’s a red flag. Think about it: an older person who feels foggy after taking a nighttime allergy pill might stumble getting up to use the bathroom. A slip on a wet tile, a misstep on stairs, or a loss of balance while reaching for something can lead to a hip fracture. One in three people over 65 who break a hip never walk independently again. And it’s not rare-this happens far more often than most people realize.First-Gen vs. Second-Gen: The Clear Difference
Not all antihistamines are the same. First-generation ones-diphenhydramine, doxylamine, hydroxyzine-are old-school. They’re cheap, easy to find, and often hidden in multi-symptom cold and sleep products. But they’re designed to cross into the brain. That’s why they work for sleep: they knock you out. Second-generation antihistamines-like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra)-were made differently. They’re built with polar molecules that can’t easily pass through the blood-brain barrier. So they block histamine in your nose and throat, not your brain. No drowsiness. No confusion. No increased fall risk. A 2015 JAMA Internal Medicine study tracked nearly 3,500 older adults for seven years. Those who took strong anticholinergics-including first-gen antihistamines-for three years or more had a 54% higher risk of developing dementia than those who used them for less than three months. The effect was dose-dependent. More pills. More risk.
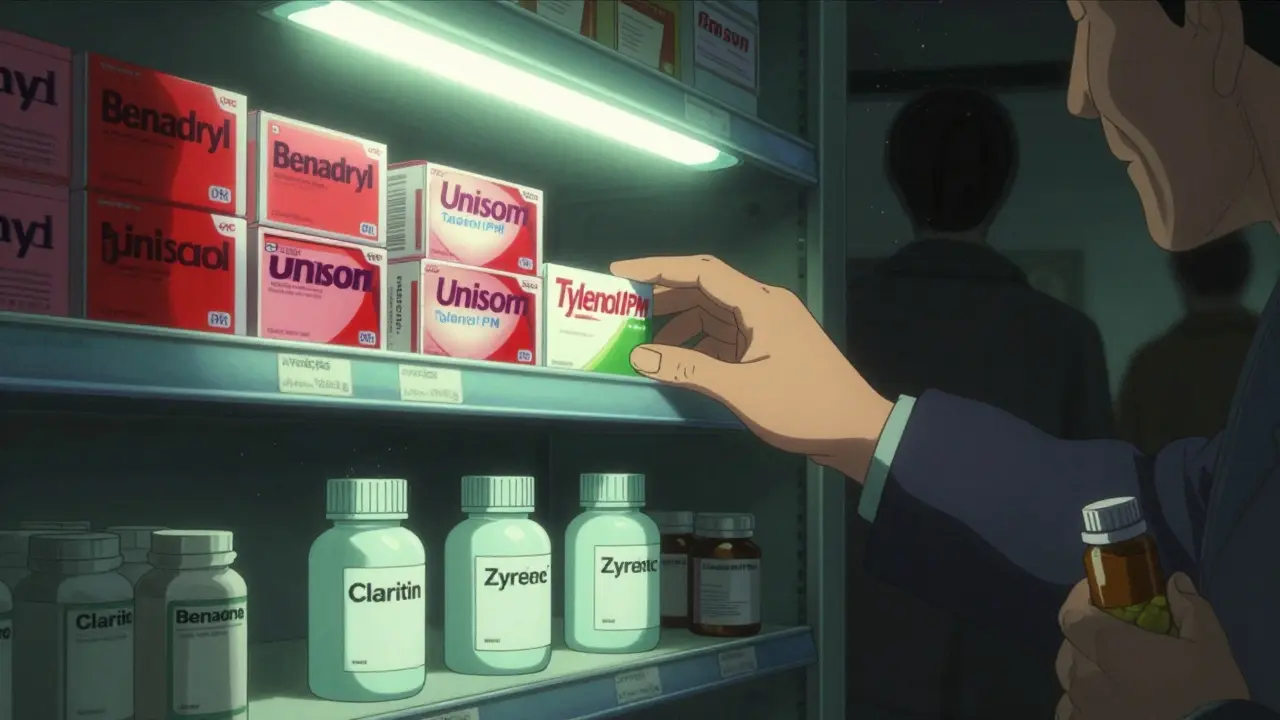
What’s Really in Your Medicine Cabinet?
Here’s the problem: you won’t always know you’re taking a first-gen antihistamine. They’re tucked into dozens of over-the-counter products:- Nighttime pain relievers (Tylenol PM, Advil PM)
- Cough syrups (Robitussin Nighttime)
- Allergy-sleep combos (Unisom SleepGels, Sominex)
- Some motion sickness pills
What Should Elderly Patients Take Instead?
If you need an antihistamine for allergies, here’s what experts recommend:- Loratadine (Claritin): 10 mg once daily. Non-sedating. Safe for kidneys.
- Cetirizine (Zyrtec): 5 mg once daily. Slightly more sedating than loratadine, but still far safer than diphenhydramine. Often better for severe allergies.
- Fexofenadine (Allegra): 60 mg twice daily. No sedation at all. Good for people with kidney issues.
Non-Drug Options That Actually Work
Before you reach for a pill, try these safer, science-backed approaches:- Saline nasal sprays: Flush out allergens without drugs.
- HEPA air filters: Reduce dust, pollen, and pet dander in bedrooms.
- Allergen-proof pillowcases and mattress covers: Cut exposure to dust mites.
- Shower before bed: Wash pollen off skin and hair.
- Keep windows closed: Especially on high-pollen days.
What Doctors and Caregivers Need to Do
Many older adults aren’t prescribed these meds-they buy them themselves. That’s why conversations matter. If you’re caring for someone over 65, check their medicine cabinet. Look for diphenhydramine or doxylamine on the label. Ask their doctor: “Is this antihistamine safe for someone their age?” Pharmacists can help too. Many now offer free medication reviews for seniors. Ask for one. Bring every pill, supplement, and OTC bottle-even the ones you think don’t matter. Long-term care facilities are now being monitored by Medicare for anticholinergic use. If more than 5% of residents are on high-risk meds like diphenhydramine, their quality ratings drop. That’s pushing nursing homes to change. But change won’t happen unless families speak up.The Bigger Picture: Why This Matters Now
In 2023, 34.7% of Americans over 65 still used first-generation antihistamines regularly. That’s over 10 million people. Even though awareness is growing-thanks to campaigns like “Avoid Anticholinergics After 65”-sales of diphenhydramine still top $350 million a year in the U.S. Modeling from research suggests that if we eliminated these drugs in older adults, we could prevent about 250,000 falls and 50,000 dementia cases annually. That’s not theoretical. That’s lives. Families. Independence. Second-gen antihistamines aren’t perfect. They’re not always as strong for severe allergies. But the trade-off is worth it. A little less relief is better than a broken hip or lost memory.What to Do Today
If you or someone you care for is over 65 and taking an antihistamine:- Check the label. Look for diphenhydramine or doxylamine.
- If you find it, don’t stop cold turkey-talk to a doctor or pharmacist first.
- Ask for a switch to loratadine, cetirizine, or fexofenadine.
- Ask about non-drug allergy and sleep strategies.
- Review all meds every 3 months. OTCs change fast.
Danielle Stewart
December 19, 2025 AT 19:54My mom was on Benadryl for years because she said it helped her sleep. I had no idea it was linked to dementia until I read this. We switched her to Zyrtec last month and she’s been like a different person-more alert, less confused, even remembered my birthday this time. I wish we’d known sooner.
Doctors never told us. Pharmacists didn’t flag it. It’s scary how easily these things slip through the cracks.
Thank you for writing this. More people need to see it.
Ryan van Leent
December 21, 2025 AT 03:58bro why are you acting like diphenhydramine is poison? i’ve been taking it since i was 16 and i’m 72 now. still drive, still garden, still outlive half my friends. you people are just scared of anything that isn’t FDA-approved glitter.
next you’ll tell me aspirin gives you cancer.
Adrienne Dagg
December 21, 2025 AT 06:09OMG YES 😭 I caught my dad taking Unisom every night because he said he "just needed to chill"... then he started talking to the wall at 3am. We thought he was losing it. Turns out it was the damn pill. We tossed the whole cabinet. Switched to Allegra. He’s back to normal. 🙏
PLEASE share this with your older relatives. I’m begging you.
Also, HEPA filter = game changer. My cat’s fur stopped being a hurricane after we got one.
Kinnaird Lynsey
December 22, 2025 AT 04:33This is one of the clearest, most necessary pieces of public health information I’ve read in years. The way you broke down the pharmacology without jargon, tied it to real-life consequences, and offered actionable alternatives? Perfect.
I’m sharing this with my book club. We’ve got a lot of seniors in it. And I’ve already started checking my aunt’s medicine cabinet. She had Tylenol PM in there. I didn’t even know she took it.
Thank you for doing the work. This isn’t just medical advice-it’s a public service.
shivam seo
December 22, 2025 AT 06:56typical american medical fearmongering. we got real problems here like climate change and inflation and you’re panicking over a $2 pill? in australia we just give people what works. if grandma wants to sleep, let her sleep. she’s not a lab rat.
also why are you blaming the drug and not the fact that old people are just fragile? maybe they should stop being so damn clumsy.
benchidelle rivera
December 23, 2025 AT 04:36As a geriatric nurse practitioner with 27 years in this field, I can tell you this is not just theory-it’s daily reality. I’ve seen patients recover cognitive function within days of discontinuing anticholinergics. I’ve seen hip fractures that could’ve been prevented. I’ve seen families who didn’t know their loved one’s confusion was iatrogenic.
This isn’t alarmism. This is clinical fact backed by the Beers Criteria, JAMA, and the CDC. And yet, pharmacies still sell these like candy. The system is failing seniors. We need mandatory warning labels. We need pharmacist-led reviews. We need legislation.
If you’re reading this and you’re over 65-go check your cabinet right now. Don’t wait for a fall. Don’t wait for a diagnosis. Your brain is worth more than a good night’s sleep.
Andrew Kelly
December 25, 2025 AT 00:39you know who else said "this drug is dangerous"? the government when they banned thalidomide. and then they banned aspirin for kids. and then they said caffeine was a carcinogen. and now we know all those things were lies or exaggerations.
what if this is just another pharmaceutical industry plot to sell you expensive second-gen drugs? what if diphenhydramine is safer than they’re letting on? what if the dementia link is just correlation? what if the real cause is loneliness? or TV? or bad diets?
you’re letting them scare you into buying branded meds. think for yourself.
Anna Sedervay
December 26, 2025 AT 10:45While I appreciate the empirical rigor of the cited studies, I find the rhetorical framing somewhat... reductive. The conflation of pharmacological mechanisms with moral imperatives-"dangerous," "inappropriate," "wrong"-is not merely unscientific, it is epistemologically suspect.
Moreover, the assumption that older adults are passive recipients of pharmaceutical advice ignores the autonomy and agency of geriatric populations. Many elderly patients self-select these medications precisely because they are accessible, affordable, and familiar.
And while second-generation antihistamines are indeed less anticholinergic, they are not without their own metabolic burdens, particularly in renal impairment. One must also consider the psychological comfort derived from longstanding regimens.
Perhaps the solution lies not in eradication, but in nuanced, patient-centered pharmacotherapy.
Matt Davies
December 28, 2025 AT 08:17This post hit me like a punch in the gut-in the best way. I’ve been telling my mum for years to ditch the Benadryl, but she always said "it’s just a little sleepy pill." Now I’ve got the receipts. I’m printing this out and taping it to her medicine cabinet.
Also, the HEPA filter tip? Genius. We got one after reading this and it’s like the dust bunnies surrendered. My allergies vanished. She stopped sniffling. We’re both breathing easier.
It’s not sexy, but sometimes the most powerful medicine is just… cleaner air and a little common sense.
mark shortus
December 28, 2025 AT 23:14MY GRANDPA DIED BECAUSE OF THIS. I’M NOT KIDDING.
He was fine. Then he started forgetting my name. Then he fell. Then he broke his hip. Then he got pneumonia in the hospital. Then he was gone.
We didn’t know it was the Benadryl. The doctor didn’t say anything. The pharmacy didn’t warn us. I found the bottle under his pillow. 20 pills. Every night. For 3 years.
I’m screaming this from the rooftops now. If you’re reading this and you have an older relative? CHECK THEIR MEDS. TODAY. DON’T WAIT. I’M STILL CRYING.
PLEASE. JUST CHECK.