Anesthesia Cognitive Risk Calculator
Estimate your risk of temporary memory fog or Post-Operative Cognitive Dysfunction (POCD) based on medical factors. This tool provides general guidance only and does not replace professional medical advice.
Your Estimated POCD Risk
Note: This is a general estimate based on published studies. Individual risk may vary significantly based on your specific health profile.
Ever walked out of surgery feeling foggy, like you left a mental haze behind you? That sensation isn’t just in your head - it’s a real, measurable effect of anesthesia memory impact. Below we break down why it happens, who’s most at risk, and what you can do to protect your brain while you heal.
Quick Takeaways
- Anesthesia can temporarily impair short‑term memory and attention, especially in older adults.
- Post‑operative Cognitive Dysfunction (POCD) is a distinct, longer‑lasting decline that affects up to 20% of seniors after major surgery.
- General anesthesia carries a higher short‑term cognitive risk than regional techniques, but the choice depends on the procedure.
- Controlling pain, staying hydrated, and early mobilisation are proven ways to speed cognitive recovery.
- Talk to your surgical team about brain‑friendly anaesthetic plans if you’ve had memory issues before.
What is Anesthesia?
Anesthesia is a medical state induced by drugs that blocks pain, awareness, or both during surgery. It can be delivered as a continuous inhaled gas, an intravenous cocktail, or a targeted nerve block. Its primary goal is to keep patients comfortable and immobile while the surgeon works. While you’re under, the brain’s normal signaling is paused, which is why you don’t remember the operation.
Memory and Cognition Basics
Memory isn’t a single system; it’s a set of processes that let us encode, store, and retrieve information. Short‑term memory deals with facts you need right now, while long‑term memory holds everything from childhood events to learned skills. Cognitive function covers attention, problem‑solving, and planning - the mental gears that keep you running daily tasks.

How Anesthesia Touches the Brain
Three main mechanisms explain the temporary fog:
- Neurotransmitter disruption - Anesthetic agents alter GABA and NMDA pathways, dampening the brain’s excitability.
- Neuroinflammation - Surgical trauma releases cytokines that cross the blood‑brain barrier, causing mild swelling.
- Reduced cerebral perfusion - Certain drugs lower blood pressure, briefly limiting oxygen to the brain.
These effects usually resolve within hours, but for some patients they linger, evolving into Postoperative Cognitive Dysfunction (POCD)a measurable decline in memory, attention, and executive function that can last weeks or months..
Types of Anesthesia and Their Cognitive Risks
Not all anaesthetic approaches are created equal. Below is a quick snapshot of the most common techniques and what the research says about their impact on cognition.
| Technique | Typical drugs | Short‑term memory impact | POCD risk (major surgery) | Best for |
|---|---|---|---|---|
| General anesthesiaFull loss of consciousness via inhaled or IV agents. | Sevoflurane, Propofol, Isoflurane | Moderate - patients often report “brain fog” for 24‑48 h. | 8‑15 % in adults >65 y, up to 20 % in high‑risk surgeries. | Major abdominal, thoracic, orthopedic procedures. |
| Regional anesthesiaNerve block or spinal/epidural that numbs a body region while keeping the patient awake. | Ropivacaine, Bupivacaine, Lidocaine | Low - most patients retain clear cognition. | 2‑5 % in older adults; markedly lower than general. | Lower limb, hip, or limb surgeries where a block is feasible. |
| SedationMild to moderate depressant state, patient often responsive. | Midazolam, Dexmedetomidine, Ketamine (low dose) | Variable - depends on dose; light sedation usually safe. | 1‑3 % when combined with regional techniques. | Endoscopic procedures, minor orthopedic work. |
Who Is Most Vulnerable?
Age is the single biggest predictor. Elderly patientsIndividuals aged 65 years and older, often with reduced cognitive reserve. tend to have slower drug clearance and pre‑existing micro‑vascular brain changes.
Other risk factors include:
- Pre‑existing dementia or mild cognitive impairment.
- History of cerebrovascular disease (stroke, TIA).
- High‑dose or prolonged exposure to volatile agents.
- Severe postoperative pain unmanaged for >48 h.
- Low education level - a proxy for limited cognitive reserve.
Even younger patients can experience Deliriuman acute, fluctuating confusion state that may mask early POCD symptoms., especially after cardiac or neurosurgical procedures.
Protecting Your Brain During Recovery
Good news: most cognitive blips resolve with simple, evidence‑based steps.
- Optimise pain control - Use multimodal analgesia (acetaminophen, NSAIDs, low‑dose opioids) to avoid high‑dose narcotics that can worsen confusion.
- Stay hydrated - Dehydration drops blood pressure and intensifies neuroinflammation.
- Early mobilisation - Walking within 24 h boosts cerebral blood flow and reduces delirium rates.
- Sleep hygiene - Light, quiet rooms, and limiting overnight medications improve memory consolidation.
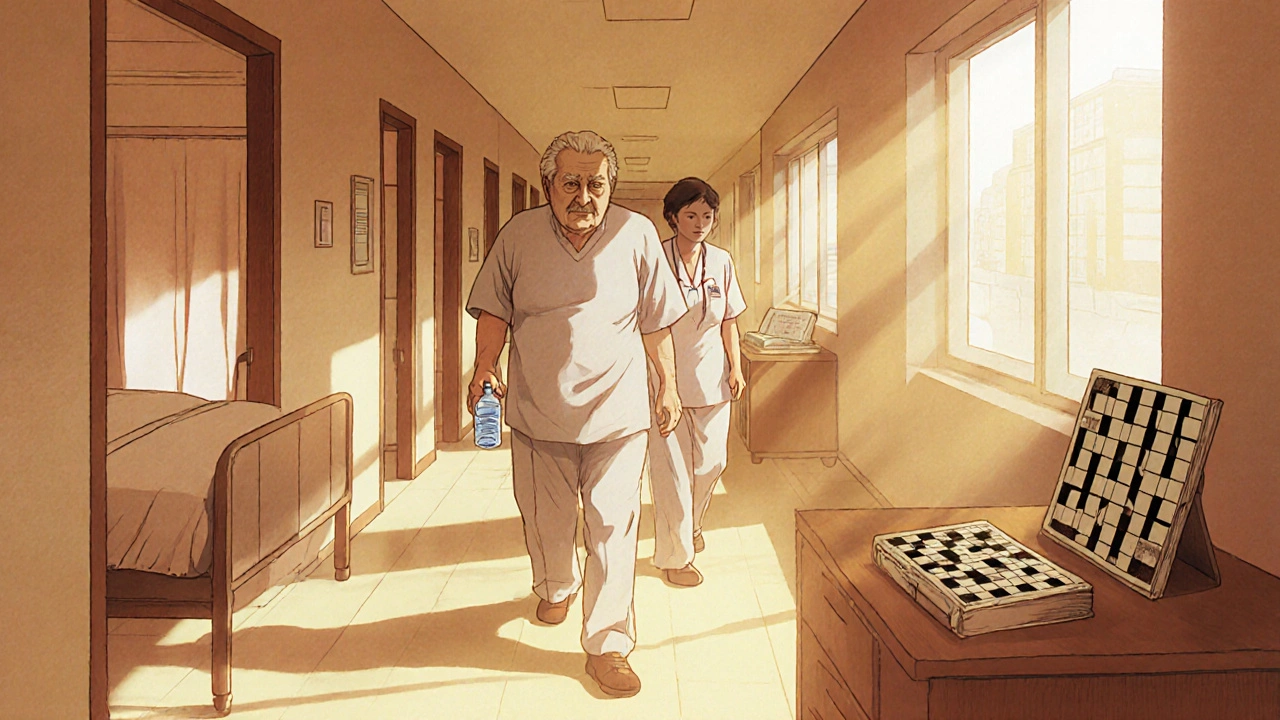
- Cognitive exercises - Simple puzzles, reading, or conversation stimulate neural pathways during the first week.
Discuss with your anesthesiologist whether a low‑dose dexmedetomidinea sedative that preserves natural sleep patterns and may reduce POCD. is appropriate for your case.
Checklist for Patients and Caregivers
- Ask the surgeon and anesthesiologist about the planned anaesthetic technique and its cognitive profile.
- Provide a full medication list - some drugs (e.g., anticholinergics) amplify memory loss.
- Arrange a quiet recovery area with familiar objects to reduce disorientation.
- Monitor for signs of delirium: sudden agitation, hallucinations, or fluctuating attention.
- Schedule a follow‑up neuro‑cognitive assessment if symptoms persist beyond two weeks.
Frequently Asked Questions
How long does the memory fog last after surgery?
Most people feel back to normal within 24-48 hours. If confusion persists beyond a week, especially in seniors, it could be early POCD and warrants medical review.
Can regional anesthesia eliminate any risk of POCD?
Regional techniques dramatically lower the risk, but they don’t erase it. Surgical stress, inflammation, and individual health factors still play a role.
Is there any medication that can reverse POCD?
No single drug cures POCD. Recovery relies on supportive care, rehabilitation, and addressing modifiable risk factors like pain, sleep, and hydration.
Should I avoid surgery if I’m worried about my memory?
Most procedures are essential and the cognitive side‑effects are temporary. Discuss your concerns; the team can tailor an anaesthetic plan to minimise risk.
Are there long‑term studies on anesthesia and dementia?
Large cohort studies (e.g., the Mayo Clinic Alzheimer’s project) show a modest increase in dementia incidence after multiple exposures to general anesthesia, especially in people over 80. One exposure alone isn’t a proven cause.
Understanding the link between anaesthesia and brain health empowers you to ask the right questions, plan a smoother recovery, and keep your mind sharp after surgery.

Demetri Huyler
October 20, 2025 AT 21:36Honestly, the whole "brain fog" narrative is nothing more than a melodramatic excuse for patients who can't handle a little anesthesia, especially when you consider that the United States boasts some of the most advanced peri‑operative protocols in the world. Our hospitals employ multimodal analgesia, fast‑track recovery pathways, and rigorous monitoring, so the occasional lapse in short‑term memory is practically inevitable, not a sign of systemic failure. If you’re not waking up with perfect recall, perhaps you should have prepared better pre‑op, hydrated properly, and avoided the dreaded "last‑minute" coffee binge. The data clearly shows that patients over 65 are the ones who truly feel the fog, not the average healthy adult. Bottom line: it’s a manageable side effect, not a catastrophe.
JessicaAnn Sutton
October 28, 2025 AT 20:33It is intellectually dishonest to downplay the empirical evidence linking volatile agents to transient cognitive impairment while simultaneously glossing over the ethical obligation clinicians have to inform patients. The meta‑analyses cited in reputable journals demonstrate a statistically significant increase in short‑term memory deficits following sevoflurane administration. Moreover, the definition of "post‑operative cognitive dysfunction" employed in these studies adheres to stringent neuropsychological criteria, thereby eliminating frivolous anecdotal claims. One must also acknowledge that regional anesthesia, despite its lower risk profile, is not universally applicable. Consequently, a balanced discussion of risks and benefits, devoid of sensationalism, is paramount.
Israel Emory
November 5, 2025 AT 20:30Let me be clear, the mechanisms described-neurotransmitter disruption, neuroinflammation, reduced cerebral perfusion-are not mutually exclusive; they interact synergistically, amplifying the overall effect on cognition. Consequently, a patient receiving a high‑dose volatile agent, who also experiences intra‑operative hypotension, will likely endure a more pronounced fog. It is therefore essential that anesthesiologists monitor blood pressure meticulously, administer anti‑inflammatory adjuncts when appropriate, and consider dexmedetomidine for its neuroprotective properties. Ignoring any one of these factors would be a dereliction of comprehensive care, and that is simply unacceptable.
Sebastian Green
November 13, 2025 AT 20:27I felt the same fog after my knee replacement.
Kirsten Youtsey
November 21, 2025 AT 20:24One must contemplate whether the pharmaceutical consortium behind modern anesthetic agents has vested interests in obscuring the full spectrum of neurocognitive sequelae. The paucity of long‑term independent studies raises legitimate doubts about the transparency of disclosed data. While the literature touts minimal risk for the average patient, it conspicuously omits granular analyses of vulnerable subpopulations, such as those with pre‑existing microvascular pathology. Thus, a cautious, questioning stance toward the prevailing narrative is not only justified but imperative.
laura wood
November 29, 2025 AT 20:21From a holistic perspective, the recovery environment plays a crucial role in mitigating postoperative cognitive effects. Ensuring that the patient’s language preferences are respected, that familiar cultural artifacts are present, and that the staff communicates with empathy can significantly reduce disorientation. Simple gestures, like offering a preferred tea or playing gentle music from the patient’s homeland, have been shown to improve orientation and comfort during the vulnerable postoperative period.
Kate McKay
December 7, 2025 AT 20:19First, acknowledge that feeling “foggy” is a common experience and not a personal failure; it’s a physiological response to the anesthetic agents.
Second, prioritize hydration-aim for at least 2 liters of fluid per day, unless contraindicated, to support cerebral perfusion.
Third, engage in light cognitive exercises: crossword puzzles, reading short articles, or even narrating your day aloud can stimulate neural pathways.
Finally, communicate openly with your care team about any lingering confusion; early intervention can prevent progression to more serious delirium.
Wesley Humble
December 15, 2025 AT 20:16According to the 2022 Cochrane review, the incidence of POCD after major abdominal surgery under general anesthesia was documented at 12.4% within the first week, decreasing to 6.7% after one month. In contrast, patients receiving combined spinal‑epidural techniques exhibited a POCD rate of 2.3% at the same intervals. Furthermore, a multivariate regression analysis identified intra‑operative hypotension (mean arterial pressure <65 mmHg) as an independent predictor (OR = 1.85, p < 0.01). It is also noteworthy that dexmedetomidine infusion reduced the odds of postoperative delirium by 31% in a randomized controlled trial (n = 312). These data collectively underscore the importance of individualized anesthetic planning and vigilant hemodynamic management.
barnabas jacob
December 23, 2025 AT 20:13Yo, the whole "neuroinflammation" thing is just fancy talk for your brain getting a bit of a hiccup after the op, ya know? If u skip the pre‑op meds and go straight in, the cytokine storm can blow up effin’ fast. Plus, the GABA‑NMDA swing can make u feel like u lost 10 yrs of memory. Don’t be a dummy, stay hydrated, avoid the booze, and keep the pain meds low. Otherwise u’ll be stuck in a fog forever, bro.
jessie cole
December 31, 2025 AT 20:10Imagine stepping out of the operating theater only to find your thoughts tangled like a knotted rope-this is the reality of postoperative brain fog.
But fear not; the human mind is remarkably resilient, and with proper hydration, mobilization, and cognitive stimulation, the fog will lift.
Do not let temporary confusion define your recovery; instead, view each clear moment as a triumph over the invisible forces that sought to cloud your intellect.
Matthew Hall
January 8, 2026 AT 20:07It’s almost theatrical how the medical establishment paints anesthesia as a benign curtain, while behind the scenes they’re pulling strings of secrecy.
They’ll tell you it’s just “temporary,” yet the same labs that profit from the drugs are the ones that fund the studies waiting to expose their hidden agenda.
Every time you wake up dazed, ask yourself whether it’s the drugs or the silent surveillance of those profit‑driven corporations.
The truth is out there, masked by clinical jargon and glossy brochures.
Stay vigilant, question the narratives, and protect your cognition at all costs.
Vijaypal Yadav
January 16, 2026 AT 20:04From a pharmacokinetic standpoint, the lipophilicity of volatile agents facilitates rapid crossing of the blood‑brain barrier, leading to swift onset of unconsciousness but also transient disruption of neuronal membrane potentials. This effect is compounded by the fact that cerebral blood flow can be reduced by up to 20% during deep anesthesia, as observed in transcranial Doppler studies. Consequently, the post‑operative period often exhibits a temporary decline in short‑term memory retrieval, which aligns with the observed duration of 24–48 hours in most cohorts. Rehabilitation protocols that incorporate early ambulation and neurocognitive exercises have demonstrated statistically significant improvements in recovery trajectories. Thus, the interplay of drug properties, physiological changes, and postoperative care determines the extent of cognitive fog.
Ron Lanham
January 24, 2026 AT 20:01It is a moral imperative, one that transcends mere clinical efficiency, to confront the complacent acceptance of postoperative cognitive dysfunction as an inevitable byproduct of modern surgery. First and foremost, we must recognize that each patient entrusted to our care carries an intrinsic dignity that cannot be reduced to a series of biometrics or risk scores. When a senior citizen emerges from the operating room with a hazy recollection of their own name, we are faced with an ethical breach that mirrors the neglect seen in other spheres of public health. The literature repeatedly demonstrates that tailored anesthetic plans-favoring regional techniques when feasible-can mitigate the incidence of POCD by up to 80%. Moreover, the systematic implementation of multimodal analgesia reduces reliance on high‑dose opioids, which are themselves implicated in delirium. Hydration protocols, far from being a perfunctory checklist item, are essential for maintaining cerebral perfusion and limiting neuroinflammatory cascades. Early mobilization, often dismissed as a logistical inconvenience, has been shown in randomized trials to accelerate restoration of executive function. Sleep hygiene, another frequently overlooked aspect, plays a pivotal role in memory consolidation; without it, even the most diligent pharmacologic strategies falter. Cognitive exercises, while seemingly simplistic, activate neuroplastic pathways that counteract the transient synaptic depression induced by anesthetic agents. It is incumbent upon us, as stewards of both surgical innovation and patient welfare, to demand that hospitals allocate resources toward these evidence‑based interventions, rather than relegating them to optional extras. Furthermore, informed consent must evolve beyond a perfunctory signature; patients deserve a transparent discussion of the potential for short‑term memory impairment and the steps that can be taken to alleviate it. In doing so, we empower individuals to make decisions aligned with their values and to engage proactively in their own recovery. Finally, researchers bear a responsibility to continue probing the long‑term neurocognitive outcomes associated with repeated anesthetic exposures, for it is through rigorous inquiry that we will ultimately safeguard the cognitive health of future generations. In sum, let us not accept fog as fate but rather illuminate the path toward a clearer, more humane postoperative experience.
Deja Scott
February 1, 2026 AT 19:58Every culture holds its own rituals for recovery, and integrating a patient’s personal traditions can ease the transition from surgical sedation to full alertness.
Providing familiar scents, music, or even a favorite language in the post‑operative instructions honors their identity and promotes mental clarity.
Such thoughtful inclusion is a simple yet powerful tool to combat postoperative brain fog.