Colchicine-Antibiotic Safety Checker
Check Your Medication Safety
This tool helps you determine if an antibiotic is safe to take with colchicine. Select your current or prescribed antibiotic and see if it's safe to use together.
Select an antibiotic and click "Check Safety" to see if it's safe to take with colchicine.
Important: This tool shows the general safety profile. Always consult your doctor before changing medications.
Colchicine is a cheap, old drug. Used for centuries to treat gout, it’s now prescribed for heart conditions, pericarditis, and even some autoimmune flare-ups. But here’s the catch: if you’re taking colchicine and your doctor prescribes a common antibiotic like clarithromycin or erythromycin, you could be walking into a life-threatening situation - and most people have no idea.
Why This Interaction Isn’t Just a ‘Possible Risk’
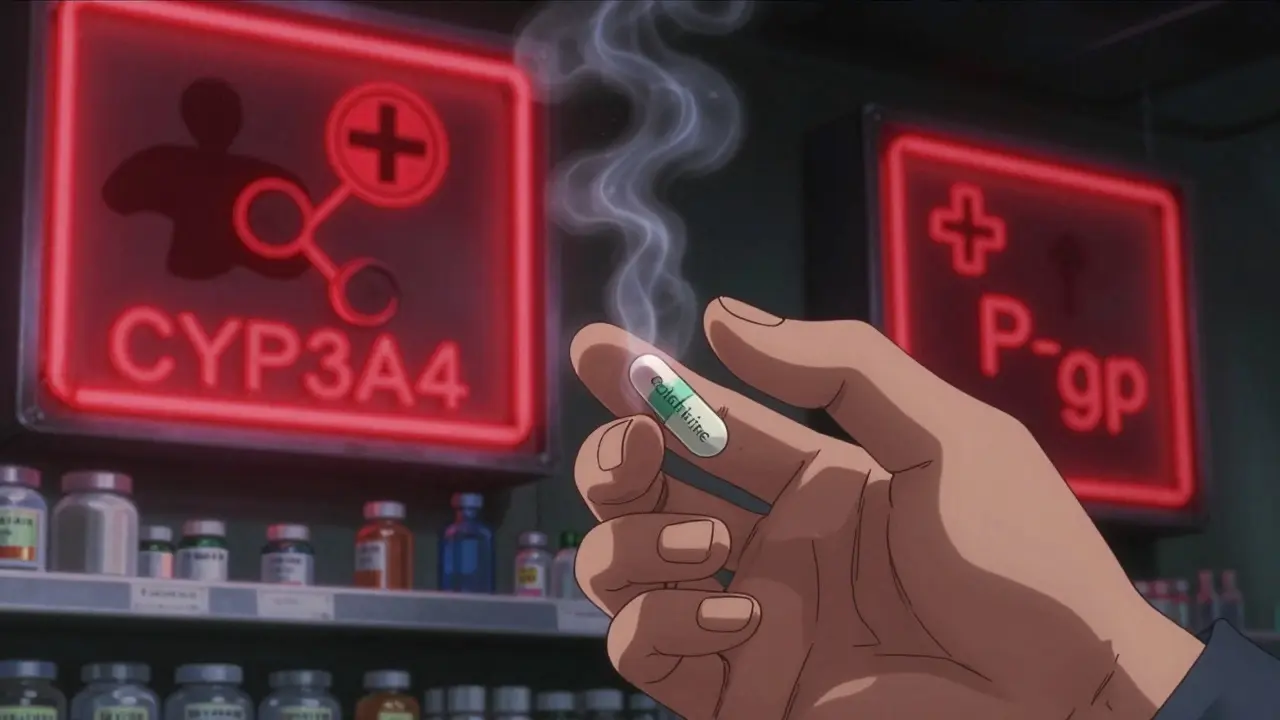
Colchicine doesn’t just sit in your body and do its job. It’s constantly being pushed out of cells by a protein called P-glycoprotein (P-gp) and broken down by an enzyme called CYP3A4 in your liver and gut. Both of these systems act like safety valves. When they’re working right, colchicine levels stay low enough to be safe.
But macrolide antibiotics like clarithromycin and erythromycin? They shut both valves down at once. Clarithromycin is a powerful inhibitor of both CYP3A4 and P-gp. When it’s in your system, colchicine can’t be cleared properly. Its concentration in your blood can jump by 2 to 4 times. That’s not a small change. It’s the difference between a medicine that helps and one that kills.
The FDA issued a black box warning for this exact reason in 2010. Black box warnings are reserved for the most dangerous drug interactions - the kind that cause death. And it’s not theoretical. From 2015 to 2020, the FDA’s own database recorded 147 cases of colchicine toxicity linked to macrolide use. Nearly two-thirds involved clarithromycin. Three people died in a single case series just from standard doses of both drugs.
Not All Macrolides Are the Same
Here’s where things get confusing. Not every antibiotic in the macrolide family is dangerous with colchicine. Azithromycin? It barely touches CYP3A4 or P-gp. Studies show it doesn’t raise colchicine levels at all. So if you need an antibiotic while on colchicine, azithromycin is your safe bet.
But clarithromycin? Avoid it. Erythromycin? Still risky. Even though erythromycin is a weaker CYP3A4 inhibitor than clarithromycin, it still blocks P-gp enough to be dangerous. And doctors don’t always know the difference. A 2023 survey of 245 physicians found that 68% had seen at least one case of colchicine toxicity from a macrolide interaction. Emergency room doctors saw it more often - 82% of them - because that’s where the damage becomes obvious.
The problem isn’t just antibiotics. Other drugs like diltiazem, verapamil, ketoconazole, and even some statins can do the same thing. But macrolides are the most common offenders because they’re prescribed so often - for sinus infections, bronchitis, pneumonia. And patients rarely connect the dots.
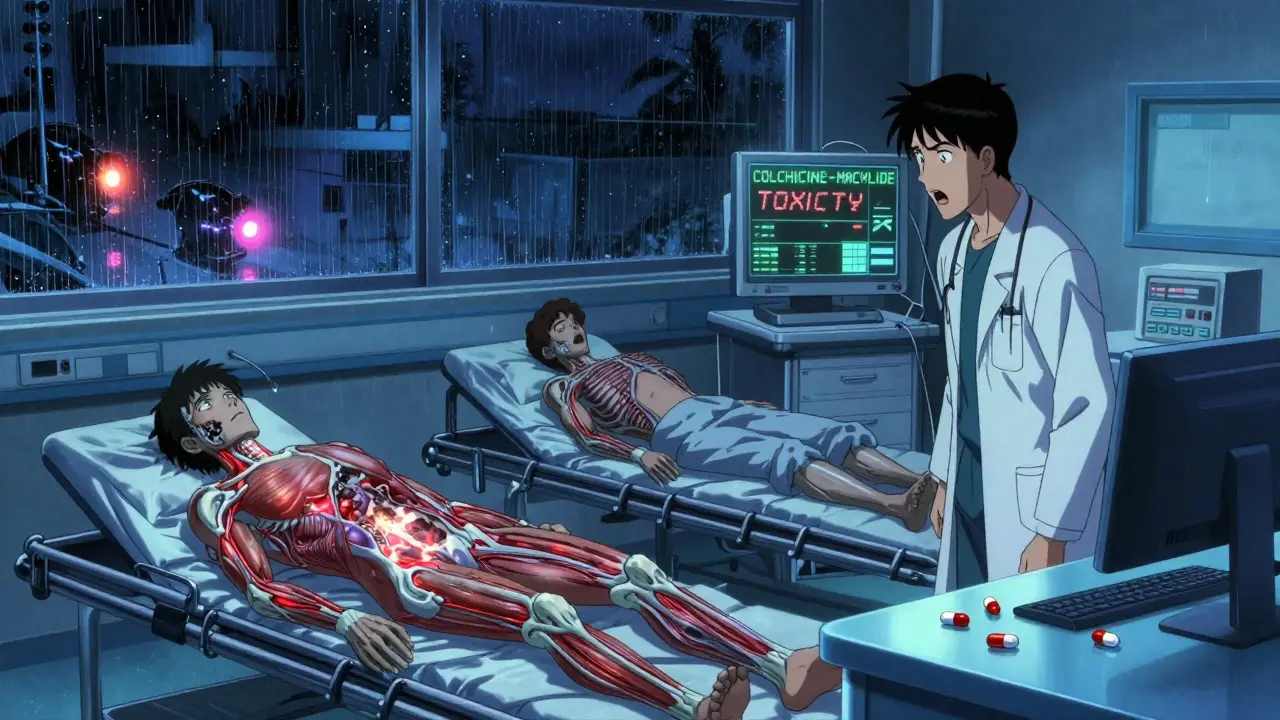
What Happens When Colchicine Builds Up
Too much colchicine doesn’t just cause nausea. It attacks your bone marrow, your muscles, your kidneys, your liver. Toxicity looks like:
- Severe diarrhea and vomiting
- Unexplained muscle pain or weakness
- Fever, fatigue, confusion
- Low white blood cell count (neutropenia)
- Low platelets and red blood cells (pancytopenia)
- Rhabdomyolysis - muscle breakdown that can fry your kidneys
- Multi-organ failure
These symptoms often show up 1 to 3 days after starting the antibiotic. By then, it’s too late for simple fixes. The 2019 case series in the Journal of Clinical Pharmacy and Therapeutics showed 12 patients with severe toxicity after taking colchicine and clarithromycin together. Three died. All were on standard doses. None were overdosing. They just didn’t know the two drugs were a deadly combo.
Why Doctors Miss This
It’s not that doctors are careless. It’s that the system fails them.
Electronic health records often don’t flag this interaction properly. A 2024 study in JAMA Internal Medicine found that when Epic updated its alert system to be more specific about colchicine-macrolide risks, inappropriate prescribing dropped by 63%. Before that, alerts were too vague - they’d pop up for every possible interaction, so doctors learned to ignore them.
Patients don’t tell doctors about all their meds. They forget about over-the-counter supplements. Some herbal products - like St. John’s wort or grapefruit juice - also inhibit CYP3A4. And many patients don’t realize colchicine is a drug that needs careful management. They think, “It’s just for gout. It’s harmless.”
Even training gaps exist. A 2021 study showed that 43% of internal medicine residents couldn’t identify high-risk drug combos involving colchicine. After targeted education, that number dropped to 13%. That’s progress - but it means nearly 1 in 5 new doctors still don’t know the risk.
What Should You Do If You’re on Colchicine?
If you’re taking colchicine for gout, heart disease, or pericarditis, here’s what you need to do right now:
- Check your current antibiotics. If you’re on clarithromycin or erythromycin, ask your doctor if you can switch to azithromycin. It works just as well for most infections and doesn’t interfere.
- Don’t start any new meds without checking. This includes OTC painkillers, sleep aids, or herbal supplements. Even common ones like turmeric or green tea extract can affect CYP3A4.
- Know your kidney function. Colchicine is cleared by the kidneys. If your kidneys are weak - even slightly - your risk of toxicity skyrockets. Ask for a simple blood test (creatinine and eGFR) if you haven’t had one in the last year.
- Ask about dose reduction. If you must take a moderate inhibitor like diltiazem or fluconazole, your colchicine dose should be cut in half. Don’t assume your doctor knows - bring this up.
And if you’re already taking colchicine and a macrolide together? Stop the antibiotic. Call your doctor immediately. Don’t wait for symptoms. Early intervention saves lives.
The Bigger Picture: Why This Matters
Colchicine use has exploded since 2010. It’s now prescribed for heart attack recovery and recurrent pericarditis - conditions affecting millions. Meanwhile, macrolides are still among the top 10 most prescribed antibiotics in the U.S. With 55 million macrolide prescriptions filled each year, and colchicine use up 217% since 2010, an estimated 1.2 million Americans are at risk of this interaction annually.
There are alternatives. Canakinumab, a biologic drug for heart inflammation, doesn’t interact with antibiotics. But it costs $198,000 a year. Colchicine costs $4,200. So we keep using it - which means we have to get better at managing its risks.
Research is moving forward. Takeda is testing a new version of colchicine - COL-098 - that doesn’t bind to P-gp. Early trials show it’s 92% less likely to interact with clarithromycin. And genetic testing is becoming more accessible. People with certain gene variants (CYP3A5*3/*3 or ABCB1 3435C>T) are 78% more likely to have toxicity. In the future, we might test for these before prescribing colchicine at all.
Bottom Line: Don’t Guess. Ask.
This isn’t a rare side effect. It’s a predictable, preventable tragedy. The science is clear. The warnings are loud. The deaths are documented.
If you’re on colchicine, don’t assume your antibiotic is safe. Don’t rely on your pharmacist to catch it. Don’t wait for an alert. Ask your doctor: “Is this antibiotic safe with colchicine?” If they say yes, ask which one. If they say clarithromycin or erythromycin, push back. Demand azithromycin instead.
Colchicine saves lives. But only if it’s used right. And that starts with knowing the danger - and speaking up before it’s too late.
Can I take azithromycin with colchicine?
Yes. Azithromycin does not significantly inhibit CYP3A4 or P-glycoprotein, so it does not raise colchicine levels. It’s the safest macrolide option if you’re taking colchicine. Many doctors now default to azithromycin for patients on colchicine to avoid dangerous interactions.
What if I accidentally took clarithromycin with colchicine?
Stop the clarithromycin immediately. Call your doctor or go to the ER. Do not wait for symptoms. Even if you feel fine, colchicine toxicity can develop over 1-3 days. Blood tests for creatinine, CK (muscle enzyme), and complete blood count are critical. In severe cases, you may need IV fluids, activated charcoal, or even dialysis.
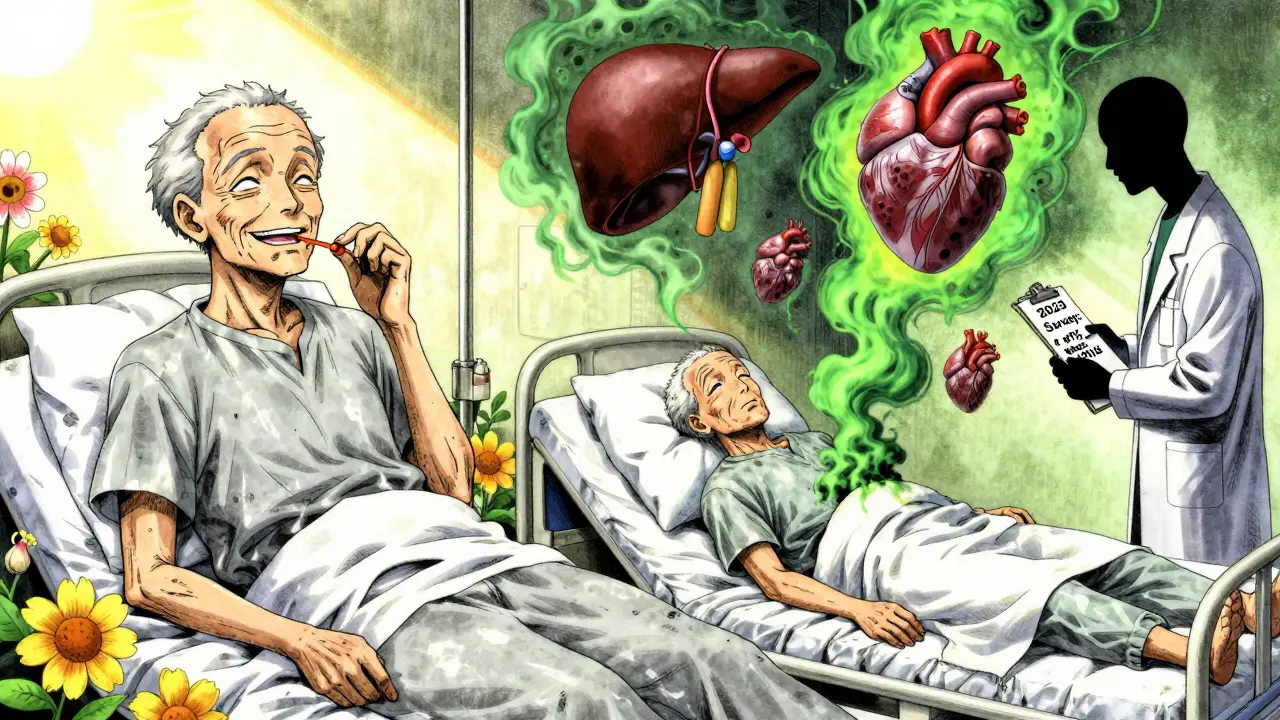
Is colchicine toxicity reversible?
It can be - if caught early. Stopping the interacting drug and supporting organ function (fluids, electrolytes, monitoring) often leads to recovery. But if toxicity progresses to rhabdomyolysis, multi-organ failure, or severe bone marrow suppression, the damage can be permanent or fatal. About 1 in 5 cases of severe toxicity result in death, especially in older adults or those with kidney problems.
Can I take ibuprofen or acetaminophen with colchicine?
Yes. Neither ibuprofen nor acetaminophen inhibits CYP3A4 or P-gp significantly. They’re safe to use with colchicine for pain or fever. But avoid NSAIDs like naproxen if you have kidney issues, as they can add to kidney strain. Always check with your doctor if you’re on multiple medications.
Do I need blood tests while taking colchicine?
Not routinely - but you should have them if you’re on other interacting drugs, have kidney disease, or are over 65. A basic blood panel (CBC, creatinine, CK) every 3-6 months is a good safety net. If you start a new antibiotic or heart medication, get tested within a week. There’s no substitute for monitoring when you’re on a drug with a narrow safety margin.
Are there any new colchicine alternatives coming?
Yes. Takeda is testing COL-098, a modified version of colchicine that doesn’t interact with P-gp. Early trials show it’s 92% safer when combined with clarithromycin. It’s still in Phase I, but if successful, it could replace standard colchicine within 5-7 years. Until then, sticking to azithromycin and avoiding strong inhibitors remains the best strategy.
Swapneel Mehta
December 20, 2025 AT 16:20This is one of those silent killers in medicine that no one talks about. I’ve been on colchicine for years for gout and had no idea clarithromycin could be this dangerous. Thanks for laying it out so clearly. I’m already texting my doctor to switch my next antibiotic to azithromycin.
Cameron Hoover
December 22, 2025 AT 08:38Wow. Just… wow. I’m a nurse and I’ve seen three patients crash from this exact combo. One was 72, on colchicine for pericarditis after a heart attack, got clarithromycin for a sinus infection. Ended up in the ICU with rhabdomyolysis. He didn’t make it. This isn’t theoretical. It’s happening every day in hospitals across America. Why aren’t we screaming about this?
Stacey Smith
December 22, 2025 AT 21:14So the government lets Big Pharma sell a $4,200 drug that kills people when paired with a $10 antibiotic, but won’t fund a safer version? Classic. They’d rather bury the data than fix the system.
Michael Ochieng
December 23, 2025 AT 09:15I’m from Kenya and we use colchicine all the time for gout. We don’t have the luxury of fancy EHR alerts, but we teach this interaction early in med school. Azithromycin is always the default. Maybe the U.S. needs less tech and more basic pharmacology training. We don’t need AI to tell us not to mix two deadly drugs.
Erika Putri Aldana
December 24, 2025 AT 05:39Why are we even still using colchicine? It’s basically poison. Why not just give people canakinumab? The drug companies don’t want us to know it’s cheaper to kill people than to make a safer version. Wake up.
Sandy Crux
December 24, 2025 AT 19:12It’s… fascinating… how the medical-industrial complex… perpetuates… these… preventable… tragedies… through… structural… inertia… and… a… willful… ignorance… of… pharmacokinetic… principles…
Hannah Taylor
December 25, 2025 AT 09:43you know what else blocks cyp3a4? 5g of weed. and the fda lets that be sold everywhere. but colchicine + clarithromycin = death? conspiracy. they want you scared so you’ll take the $198k drug. they’re lying.
Jason Silva
December 25, 2025 AT 19:16Bro… this is wild 😳 I just got prescribed clarithromycin last week for my sinus infection… and I’ve been on colchicine for 3 years… I’m calling my doctor right now. Thanks for the heads up. Y’all saved my life. 🙏
mukesh matav
December 26, 2025 AT 01:43My uncle died from this in 2018. He was 68. Took colchicine and erythromycin for a cough. No one warned him. No one warned the doctor. We found out too late. This needs to be on every prescription label.
Peggy Adams
December 26, 2025 AT 06:37they’ve been hiding this for years. if you search ‘colchicine death’ on google, the first 10 results are all pharma ads. that’s not a coincidence. they’re burying the truth.
Theo Newbold
December 27, 2025 AT 16:46Let’s be real: the only reason this isn’t a class-action lawsuit is because the victims are mostly elderly, low-income, and don’t know how to sue. The system is designed to let this happen. This isn’t negligence. It’s profit-driven negligence.
Jay lawch
December 29, 2025 AT 11:19India has over 50 million people on colchicine. We don’t have access to azithromycin in rural areas. We use erythromycin because it’s cheaper. So what do we do? Let them die? Or do we push for a national policy to subsidize azithromycin for colchicine users? The answer is obvious. But the government won’t act until a thousand more die. And they will. Because profit > people. Again.
Christina Weber
December 30, 2025 AT 08:23Correction: The FDA issued the black box warning in 2010, not 2011. Also, the 2023 survey cited was published in JAMA Network Open, not JAMA Internal Medicine. And azithromycin’s half-life is 68 hours, not 48 - this matters for dosing intervals. Accuracy matters in medical communication. Please fact-check before posting.