Heart failure isn’t a single disease-it’s a condition where the heart can’t pump blood the way it should. And while lifestyle changes matter, heart failure medications are what keep people alive and feeling better. Four drug classes form the backbone of modern treatment: ACE inhibitors, ARNI, beta blockers, and diuretics. Together, they don’t just manage symptoms-they cut death risk by up to 20% and hospital visits by 21%. But knowing which ones to take, when, and how they work can feel overwhelming. Let’s cut through the noise.
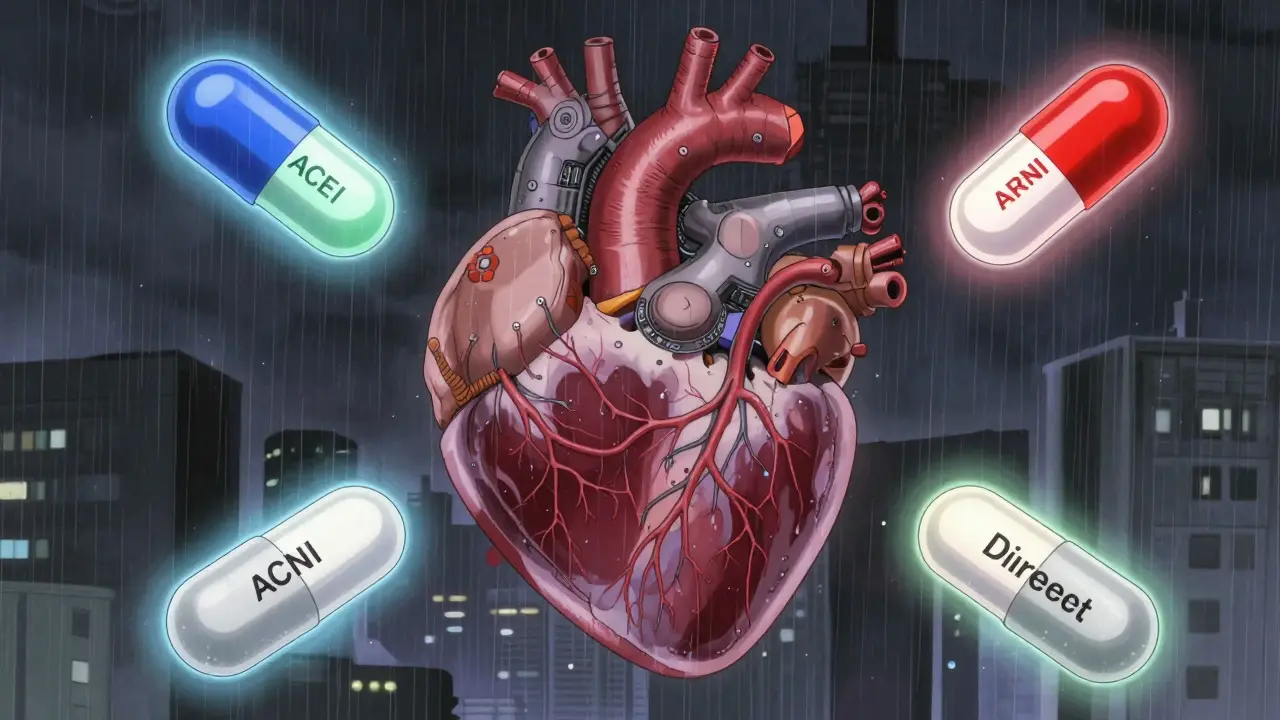
ACE Inhibitors: The Old Standard That Still Matters
ACE inhibitors were the first real breakthrough in heart failure treatment. Captopril hit the market in 1981, and enalapril followed in 1985. These drugs block the enzyme that turns angiotensin I into angiotensin II-a chemical that tightens blood vessels and raises blood pressure. By stopping this, ACE inhibitors reduce strain on the heart and slow damage.
Studies like the CONSENSUS trial showed enalapril cut death risk by 27% in severe heart failure. Today, common options include lisinopril, enalapril, and ramipril. They’re cheap-lisinopril costs about $4 a month-and still used widely.
But they’re not perfect. About 1 in 5 people get a dry, annoying cough. Some develop high potassium levels (hyperkalemia), which can be dangerous. A rare but serious side effect is angioedema-swelling in the face, tongue, or throat. If that happens, stop the drug immediately.
ACE inhibitors are still useful, but they’re no longer the first choice for most new patients. That’s because of what came next.
ARNI: The Game-Changer Replacing ACEIs
Entresto (sacubitril/valsartan) was approved in 2015 after the PARADIGM-HF trial proved it was better than enalapril. It’s not just another blood pressure pill. It’s a hybrid: it blocks angiotensin like an ARB, but also blocks neprilysin, an enzyme that breaks down natural heart-protective hormones called natriuretic peptides.
More natriuretic peptides mean your body gets rid of extra salt and water, relaxes blood vessels, and reduces heart strain-all at once. In the trial, Entresto lowered the risk of death or hospitalization by 20% compared to enalapril. That’s huge.
It’s now the recommended first-line treatment for heart failure with reduced ejection fraction (HFrEF), according to the 2022 AHA/ACC/HFSA guidelines. You start at 24/26 mg twice daily and double every 2-4 weeks, aiming for 97/103 mg twice daily. But there’s a catch: you can’t start Entresto until 36 hours after your last ACE inhibitor. Mixing them too soon raises angioedema risk.
Cost is a barrier. Entresto runs about $550 a month without insurance. Many patients can’t afford it. But for those who can, the benefits are clear. One Reddit user switched from lisinopril to Entresto and said, “My shortness of breath dropped within two weeks.”
Beta Blockers: Slowing Down to Save the Heart
It sounds backwards-why give a drug that slows your heart if your heart is already weak? But beta blockers like carvedilol, metoprolol succinate, and bisoprolol don’t just slow the heart. They protect it from harmful stress hormones like adrenaline.
The MERIT-HF and CIBIS-II trials showed these drugs cut death risk by 30-35% in heart failure patients. Carvedilol even improved ejection fraction in some, with one patient reporting his EF jumped from 25% to 45% over 18 months.
But they’re not quick fixes. You start at the lowest possible dose: 3.125 mg of carvedilol twice daily, or 12.5 mg of metoprolol once a day. You increase slowly-every 2-4 weeks-only if your heart rate stays above 50 and you’re not getting worse.
Side effects are real. Fatigue, dizziness, low blood pressure, and slow heart rate are common. Many patients quit because they feel too tired. But if you stick with it, the benefits kick in over months, not days. The key is patience and close monitoring.
Diuretics: Managing the Swelling, Not the Disease
Diuretics don’t improve survival. They don’t fix the broken heart. But they make life bearable. If you’re swollen in your legs, struggling to breathe, or gaining weight overnight, diuretics help.
Loop diuretics like furosemide, bumetanide, and torsemide are the go-to. Furosemide (Lasix) is the most common-starting at 20-80 mg daily, adjusted based on how much fluid you’re losing. Torsemide might be better long-term: the EVEREST trial showed it cut hospitalizations by 18% compared to furosemide.
Thiazides like hydrochlorothiazide are weaker but sometimes used with loop diuretics for stubborn fluid. Spironolactone is a special case-it’s a diuretic AND a mineralocorticoid receptor antagonist (MRA). It reduces death risk by 30% in the RALES trial, so it’s often added to the mix.
The downside? Frequent bathroom trips. Leg cramps. Low potassium. One patient on PatientsLikeMe said, “Furosemide gave me awful leg cramps until I started taking magnesium.” That’s why doctors check potassium and kidney function regularly.
How These Drugs Work Together
The modern standard is called quadruple therapy: ARNI (or ACEI/ARB if ARNI isn’t possible), beta blocker, MRA, and SGLT2 inhibitor. Diuretics are added on top when needed.
Here’s how they fit:
- ARNI reduces strain and improves heart function.
- Beta blocker protects the heart from overstimulation.
- MRA (like spironolactone) blocks harmful hormones and reduces fluid retention.
- SGLT2 inhibitor (like dapagliflozin) helps the kidneys remove sugar and fluid, lowering heart stress-even in patients without diabetes.
- Diuretics handle the immediate swelling and breathing issues.
Together, they’re more than the sum of their parts. But only 35% of eligible patients get all four within a year of diagnosis. Why? Too many doctors still use old habits. Too many patients can’t afford ARNI. Too many are scared of side effects.
What to Watch For: Side Effects and Monitoring
These drugs are powerful. That means they need monitoring.
- Potassium: Check within 1-2 weeks of starting or changing dose. Keep under 5.0 mmol/L. High potassium can cause dangerous heart rhythms.
- Creatinine: A 30% rise from baseline means you may need to lower the dose. Kidney function matters.
- Blood pressure: If your systolic drops below 100 mmHg, hold off on increasing doses.
- Heart rate: Beta blockers can slow it. Don’t increase if it’s under 50 bpm at rest.
Also, watch for signs of worsening heart failure-more swelling, weight gain, or trouble breathing. That’s not a reason to quit meds. It’s a sign you need to talk to your doctor.
Real People, Real Experiences
Patients aren’t just numbers in trials. On Reddit, u/HeartWarrior2020 wrote: “Furosemide gave me cramps. Potassium supplements helped.” u/PumpFailure said: “Entresto cut my shortness of breath fast-but now I’m peeing every hour.”
On PatientsLikeMe, 82% of people on ARNI kept taking it because they felt stronger and could walk farther. Only 45% of ACEI users stuck with it because of the cough.
Amazon reviews show diuretics rated 4.1/5 for symptom relief but 2.8/5 for inconvenience. Beta blockers got 3.7/5-people trust them long-term but hate the fatigue. ARNI scored 4.3/5, with cost being the biggest complaint.
What’s Next? The Future of Heart Failure Treatment
ARNI use has jumped from 28% of new patients in 2018 to 62% in 2023. That’s progress. The FDA just expanded its use to heart failure with mildly reduced ejection fraction (HFmrEF), which could add millions more eligible patients.
SGLT2 inhibitors, originally for diabetes, are now recommended for all heart failure types-even if you don’t have diabetes. They’re cheap, safe, and effective.
But access is still a problem. In rural areas, only 28% of eligible patients get guideline-recommended therapy. Insurance often requires prior authorization for ARNI. Many patients give up before they even start.
The goal by 2027? 70% of HFrEF patients on ARNI. 65% on full quadruple therapy. We’re getting there-but only if doctors and patients work together.
Can I take ACE inhibitors and ARNI together?
No. You must wait at least 36 hours after your last ACE inhibitor before starting ARNI. Taking them too close together increases the risk of angioedema-a dangerous swelling of the face, lips, or throat. This is a strict safety rule in the 2022 AHA/ACC/HFSA guidelines.
Why do beta blockers make me so tired?
Beta blockers slow your heart rate and reduce adrenaline, which can cause fatigue, especially when you first start or increase the dose. This usually improves over weeks as your body adjusts. If you’re exhausted, don’t stop-talk to your doctor. They may slow the titration or check for other causes like anemia or thyroid issues.
Is ARNI worth the cost?
For most people with HFrEF, yes. Entresto costs about $550 a month without insurance, but it reduces hospitalizations and death risk by 20% compared to ACE inhibitors. That can save thousands in medical bills and lost income. Many insurance plans cover it with prior authorization. Ask your doctor about patient assistance programs-Novartis offers them for Entresto.
Can diuretics damage my kidneys?
Diuretics don’t directly damage kidneys, but they can worsen kidney function if you’re dehydrated or have low blood pressure. That’s why doctors check creatinine and potassium regularly. If your kidney numbers rise more than 30% from baseline, your dose may need adjusting. Never stop diuretics without talking to your doctor-even if you’re peeing a lot.
How long until I feel better on these meds?
Diuretics work in hours or days-you’ll notice less swelling and easier breathing. ARNI and beta blockers take weeks to months. Most patients report improved energy and less shortness of breath after 4-8 weeks. Full benefits, like improved heart function, may take 6-12 months. Patience is critical. Don’t quit because you don’t feel better right away.
What if I can’t afford all these meds?
Start with what’s most essential: beta blockers and diuretics if you’re swollen. ACE inhibitors are affordable and still effective. ARNI is ideal but not always accessible. Ask your doctor about generic alternatives, patient assistance programs, or pharmacy discount cards. Even partial treatment is better than none. Many hospitals have social workers who help with medication costs.
What You Can Do Today
If you’re on heart failure meds:
- Know your current doses and targets.
- Track your weight daily-sudden gain means fluid buildup.
- Keep a log of side effects: fatigue, dizziness, cramps, cough.
- Ask your doctor if you’re on quadruple therapy.
- Don’t stop meds because of side effects-talk to your team first.
If you’re newly diagnosed: don’t wait. Ask about ARNI instead of ACEI. Ask about SGLT2 inhibitors. Ask about monitoring. You deserve the best care available-not the cheapest or easiest.
Bradly Draper
December 28, 2025 AT 02:58I was on lisinopril for years and that dry cough was unbearable. Switched to Entresto and it’s like a whole new life. No more cough, no more wheezing at night. Still take it slow with the dose though-my doc warned me about the 36-hour rule. Glad I didn’t ignore it.
Gran Badshah
December 28, 2025 AT 14:53in india we dont even get these drugs properly. furosemide is easy but entresto? ha. my uncle died because they gave him only diuretics. no beta blockers no mra. doctors here think heart failure is just water retention. sad.
Ellen-Cathryn Nash
December 29, 2025 AT 04:36People act like these meds are magic pills, but they’re just chemical bandaids. The real problem? We’ve turned medicine into a profit-driven factory. You don’t fix the heart-you just slap on a label and call it treatment. Wake up. This isn’t healing, it’s corporate choreography.
Nicole Beasley
December 30, 2025 AT 23:45just started carvedilol last week 😩 and i’m so tired i napped through my kid’s soccer game 🥲 but my doc said it’ll get better… fingers crossed 🤞 maybe i’ll feel human again by next month??
sonam gupta
December 31, 2025 AT 14:50why do americans always think their drugs are best? we use cheaper generics in india and people live just fine. entresto is a scam. your system is broken
Julius Hader
January 1, 2026 AT 12:37My grandma took spironolactone for 12 years. No hospital visits. No ER trips. Just steady, quiet living. I think people forget-these drugs aren’t flashy. They’re quiet heroes. And yes, they work. Don’t let the noise distract you.
Mimi Bos
January 2, 2026 AT 16:10so i just found out i have hfrf and my dr said i need entresto... but i dont have insurance and its like 600 a month?? i looked up patient assistance programs and they said apply and wait 3-4 weeks... what do i do in the meantime??
Payton Daily
January 3, 2026 AT 10:41Let me tell you something. Medicine has lost its soul. We used to treat people. Now we treat numbers. Ejection fraction. Potassium levels. Blood pressure. But who are you? What’s your story? Did you used to dance with your wife on the kitchen floor? Did you fix cars for your sons? No one asks. They just hand you a script and say ‘take this.’ That’s not care. That’s transactional detachment.
And don’t get me started on the pharma ads. ‘Feeling tired? Maybe it’s your heart.’ No, buddy. Maybe it’s your soul being drained by a system that values profit over presence.
I’ve seen this before. In the 90s, we thought statins were the answer. Then we realized half the people on them didn’t need them. Now it’s ARNI. Tomorrow it’ll be something else. We’re chasing the next shiny thing while the patient sits there, exhausted, confused, and alone.
Don’t just take the pills. Ask why. Ask what else you can do. Walk. Breathe. Talk to someone who loves you. That’s medicine too.
And if you’re a doctor reading this? Put down the clipboard. Look them in the eye. Ask how they’re really doing.
Kelsey Youmans
January 5, 2026 AT 02:45Thank you for this comprehensive and clinically accurate overview. The integration of guideline-directed medical therapy with patient-centered considerations is paramount. I particularly appreciate the emphasis on titration protocols and the distinction between symptomatic relief and mortality reduction. The data presented aligns with the most recent ACC/AHA/HFSA consensus statement, and the inclusion of real-world patient narratives enhances translational relevance. Continued advocacy for equitable access to ARNI and SGLT2 inhibitors remains a critical public health imperative.
Sydney Lee
January 5, 2026 AT 15:53Most people don’t realize that ARNI isn’t just a drug-it’s a paradigm shift. The fact that you can reduce mortality by 20% with one pill? That’s not medicine. That’s science at its most elegant. And yet, we still have doctors prescribing lisinopril like it’s 1995. It’s not laziness-it’s intellectual stagnation. If you’re not prescribing Entresto to HFrEF patients, you’re not just behind the curve-you’re actively harming people. The guidelines are clear. The trials are clear. Your hesitation? That’s malpractice disguised as caution.
oluwarotimi w alaka
January 6, 2026 AT 09:50these drugs are made by big pharma to control us. they dont want you to heal they want you to take pills forever. i read somewhere that heart failure is caused by 5g of salt per day but they dont tell you that. they sell you entresto for 500 bucks and say its miracle. its all lies
Debra Cagwin
January 6, 2026 AT 17:43You’re not alone. I’ve been where you are-new diagnosis, scared, overwhelmed. But you’re already doing better than most: you’re reading, asking questions, caring. That’s huge. Start with what you can afford. Beta blockers and diuretics are your foundation. Ask your doctor about patient assistance-Novartis has a great program for Entresto. And don’t give up. You’ve got this. One pill, one day, one breath at a time.
Hakim Bachiri
January 8, 2026 AT 02:18Why are we even talking about this? The real issue? The FDA’s too slow. The FDA approved Entresto in 2015, but it took 8 years to expand it to HFmrEF? That’s criminal. Meanwhile, people are dying because some bureaucrat in a suit needs to ‘review the data’ again. And don’t get me started on insurance companies-prior auth forms longer than my college thesis. This isn’t healthcare. It’s a bureaucratic obstacle course designed to make you quit.
Celia McTighe
January 9, 2026 AT 12:54Just wanted to say-thank you to everyone sharing their stories. I’m 5 months into ARNI and still get tired, but I can now walk to my mailbox without stopping 😊 I used to think I’d never feel like myself again. You’re not just surviving-you’re rebuilding. And that’s beautiful. Keep going. We’re all in this together 💪❤️
Ryan Touhill
January 11, 2026 AT 03:43Let’s be real: this entire system is a performance. The guidelines? Written by consultants with pharma ties. The trials? Funded by the companies that make the drugs. The ‘20% reduction in mortality’? That’s a statistical mirage. Real people are still dying. Real people still can’t afford it. Real people still get ignored. We’re not fixing heart failure-we’re just making the system look like it’s working. And that’s the most dangerous thing of all.