HIV Medication-Statins Safety Checker
Check Your Statin Combination Safety
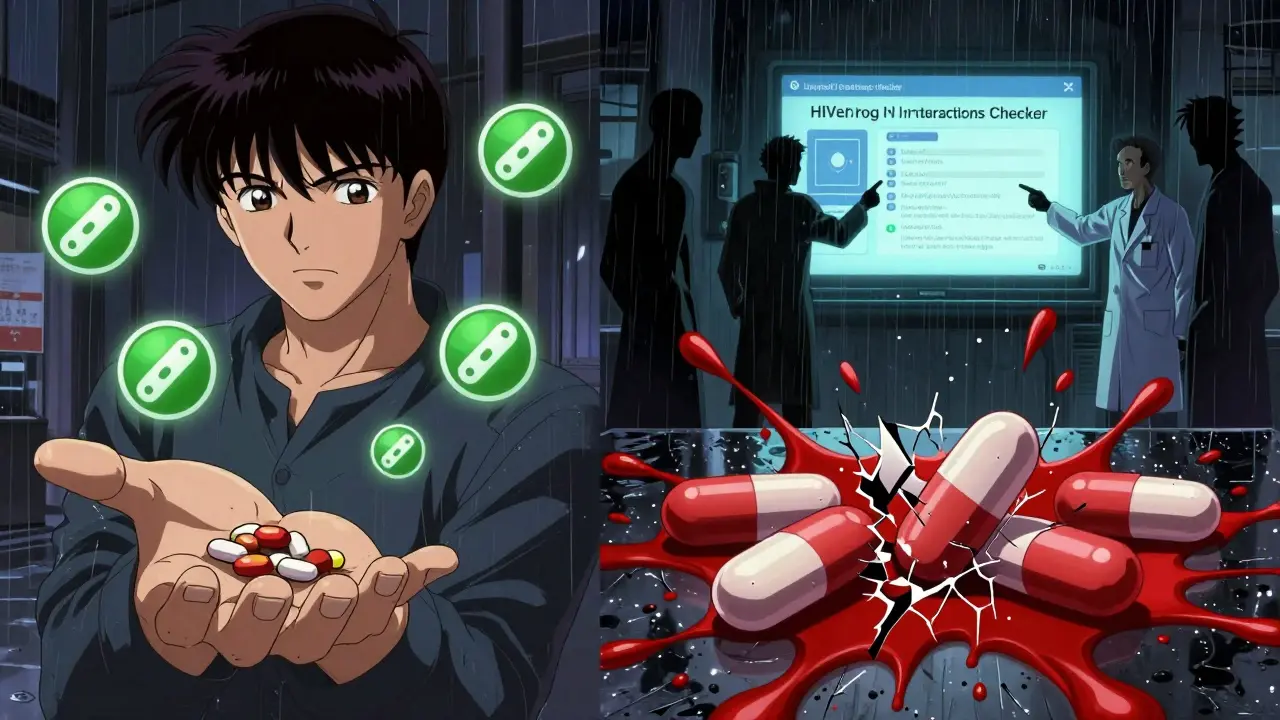
Enter your HIV medication regimen and statin to see if the combination is safe. This tool uses the latest guidelines from HIV treatment and cardiology experts.
Safety Result
Safety Status
People living with HIV are living longer than ever before. Thanks to modern antiretroviral therapy (ART), many are now managing HIV like a chronic condition-similar to high blood pressure or diabetes. But with that longer life comes a new challenge: heart disease. People with HIV have a 50% higher risk of heart attack than those without HIV, even when their virus is well controlled. That’s why statins, the go-to drugs for lowering cholesterol and protecting the heart, are increasingly prescribed. But here’s the catch: many HIV medications don’t play well with statins. Mixing the wrong ones can lead to dangerous muscle damage, kidney failure, or even death.
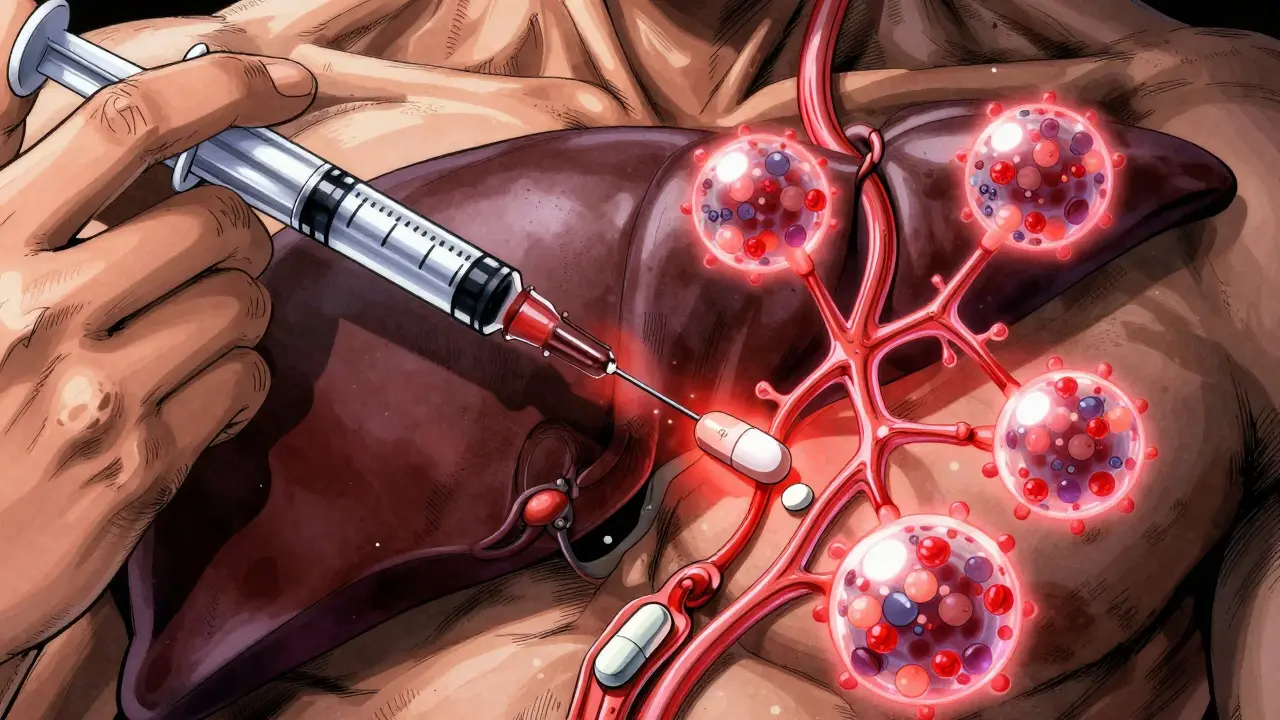
Why HIV Drugs and Statins Don’t Always Mix
The problem isn’t that statins are dangerous on their own. It’s that many HIV drugs interfere with how your body breaks them down. Most statins are processed by an enzyme called CYP3A4 in your liver. But two common HIV drug components-ritonavir and cobicistat-are powerful inhibitors of this enzyme. Think of CYP3A4 as a factory that clears statins from your bloodstream. When ritonavir or cobicistat shuts it down, statins pile up. That’s when muscle pain turns into rhabdomyolysis, a condition where muscle cells break down and flood your kidneys with toxic proteins.The numbers are alarming. When you take darunavir/cobicistat with atorvastatin, your body absorbs nearly three times more statin than normal. With simvastatin or lovastatin, levels can spike up to 20 times higher. That’s why the FDA and major health agencies have issued clear warnings: simvastatin and lovastatin are absolutely off-limits with any boosted HIV regimen. These drugs are banned for use in people on ritonavir- or cobicistat-containing HIV treatments. There’s no safe dose.
Which Statins Are Safe to Use With HIV Medications?
Not all statins are created equal. Some are broken down by different enzymes, making them much safer to pair with HIV drugs. Here’s what works:- Pitavastatin (Livalo): This is the safest choice. It’s metabolized mostly by glucuronidation, not CYP3A4. It has minimal interaction with boosted HIV drugs and is often the top pick for people on ART.
- Pravastatin (Pravachol): Also low-risk. It’s cleared by the kidneys and doesn’t rely heavily on liver enzymes. Dosing doesn’t usually need adjustment.
- Rosuvastatin (Crestor): Can be used, but only at low doses. With ritonavir or cobicistat, stick to 10 mg daily. Higher doses raise the risk of muscle damage.
- Atorvastatin (Lipitor): The most commonly used statin in HIV patients, but with strict limits. With darunavir/cobicistat, don’t exceed 20 mg per day. With unboosted regimens, 40 mg is often acceptable.
- Fluvastatin (Lescol): An option for those who can’t tolerate the others. It’s processed by CYP2C9, so it’s less affected by CYP3A4 inhibitors. But watch out-ritonavir can still raise its levels by about 2-fold.
Here’s what you should avoid:
- Simvastatin (Zocor)
- Lovastatin (Mevacor)
These two are not just risky-they’re dangerous. No exceptions. Even a single dose can be life-threatening when combined with boosted HIV drugs.
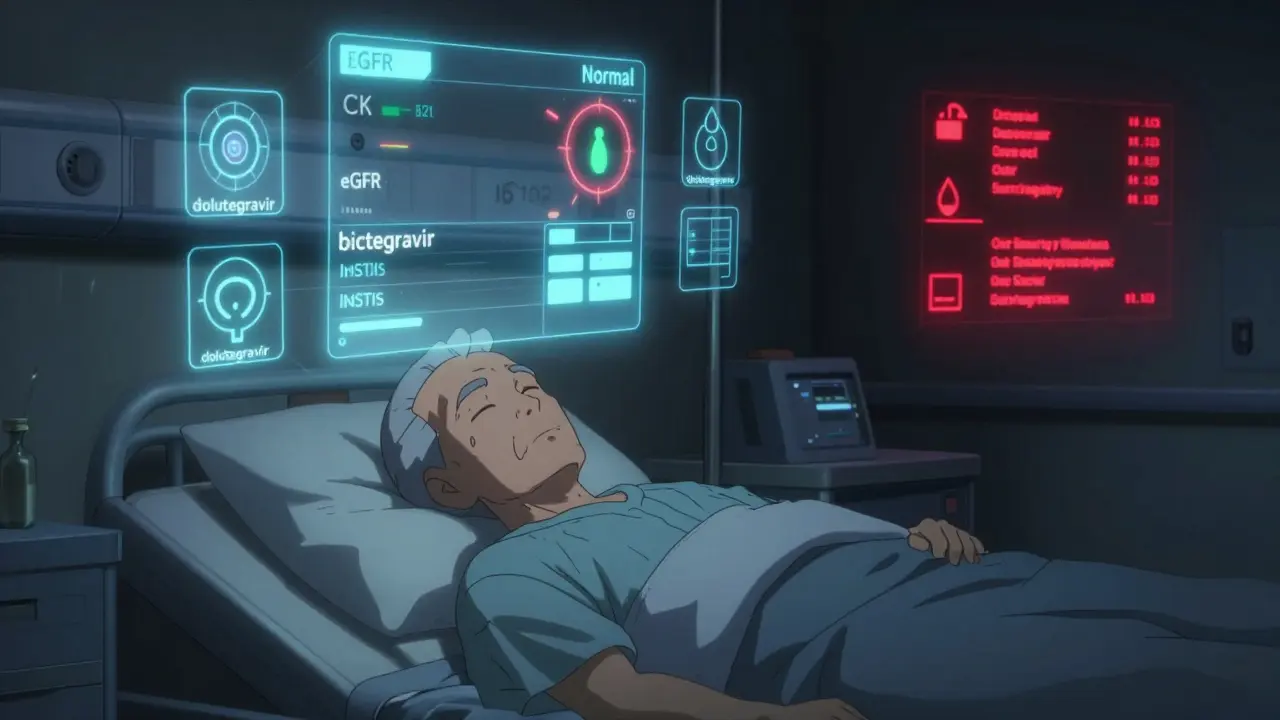
What About Newer HIV Drugs?
The good news is that newer HIV medications are much friendlier to statins. Integrase strand transfer inhibitors (INSTIs) like dolutegravir, bictegravir, and raltegravir don’t interfere with CYP3A4. That means if you’re on a regimen like Biktarvy or Dovato, you can usually take standard doses of most statins without major concerns. This is why many doctors now prefer INSTI-based regimens for patients who also need heart protection.But even with these safer HIV drugs, caution is still needed. If you’re on an INSTI and start a new medication-like a blood pressure pill, an antibiotic, or even an over-the-counter supplement-it could still affect your statin. Always check for interactions before adding anything new.
Dosing Rules You Can’t Ignore
Safe doesn’t mean “any dose.” Even with the right statin, you need to follow strict limits:- With darunavir/cobicistat: Atorvastatin max = 20 mg/day; rosuvastatin max = 10 mg/day.
- With lopinavir/ritonavir or atazanavir/ritonavir: Rosuvastatin max = 10 mg/day; atorvastatin max = 20 mg/day.
- With dolutegravir, bictegravir, or other unboosted INSTIs: Standard statin doses are usually fine (e.g., atorvastatin 40-80 mg, rosuvastatin 10-20 mg).
- With ritonavir-boosted regimens: Avoid pitavastatin above 4 mg/day unless monitored closely.
These aren’t suggestions-they’re hard limits backed by clinical trials and FDA labeling. Going over them increases your risk of muscle damage without adding any extra heart benefit.
Monitoring: What Your Doctor Should Be Checking
If you’re on both an HIV regimen and a statin, you need regular monitoring. This isn’t optional.- Baseline blood tests: Before starting a statin, your doctor should check your creatine kinase (CK) levels and liver enzymes.
- Follow-up tests: Repeat CK and liver tests within 4-6 weeks of starting or changing your statin dose.
- Watch for symptoms: Muscle pain, weakness, or dark urine are red flags. Don’t wait for a blood test-call your doctor immediately if you feel this way.
- Check kidney function: Statin-related muscle breakdown can damage your kidneys. Your doctor should monitor your creatinine and eGFR regularly.
Older adults and people with kidney disease are at higher risk. If you’re over 65 or have any kidney issues, your doctor may start you on an even lower dose.
Other Medications That Can Make Things Worse
It’s not just HIV drugs. Many other common medications can pile on the risk:- Calcium channel blockers like felodipine or verapamil (used for high blood pressure) can also block CYP3A4. If you’re on one of these, your statin dose may need to be cut even further.
- Gemfibrozil (used for high triglycerides) is extremely dangerous with statins. It increases the risk of rhabdomyolysis by up to 10-fold. If you need a triglyceride-lowering drug, choose fenofibrate or omega-3 fatty acids instead.
- Antifungals like ketoconazole or itraconazole, and some antibiotics like clarithromycin, can also interfere. Always tell your doctor what else you’re taking-even herbal supplements like St. John’s wort or red yeast rice.
What You Can Do Right Now
If you’re on HIV meds and need a statin, here’s your action plan:- Know your HIV regimen. Is it boosted (with cobicistat or ritonavir)? Or is it an INSTI-based combo like Biktarvy or Dovato?
- Don’t guess your statin. Never start a statin on your own. Ask your doctor which one is safe for your specific HIV drugs.
- Use the Liverpool HIV Drug Interactions Checker. It’s free, updated monthly, and used by doctors worldwide. Type in your exact medications and see what’s safe. Don’t rely on memory or old advice.
- Report muscle pain immediately. Even mild soreness can be an early warning sign.
- Review all your meds twice a year. Include supplements, OTC painkillers, and vitamins. Many people forget these can interact.
Why This Matters More Than Ever
In 2007, about 15% of people with HIV were on statins that were unsafe for their HIV drugs. By 2015, that number dropped to under 5%. That’s progress. But here’s the problem: only 40-60% of people who *should* be on a statin actually are. Too many are still skipping heart protection because they’re afraid of interactions-or their doctors aren’t prescribing the right ones.Heart disease kills more people with HIV than AIDS does today. You can’t ignore it. But you don’t have to choose between living with HIV and protecting your heart. The right statin, at the right dose, with the right HIV regimen, can keep you healthy for decades.
The key is precision. Not guesswork. Not luck. Not hoping nothing goes wrong. It’s knowing exactly what you’re taking and why. And using the right tools to make sure it’s safe.
Can I take simvastatin if I have HIV?
No. Simvastatin is absolutely contraindicated with all HIV protease inhibitors and cobicistat-containing regimens. Taking it with these drugs can increase statin levels up to 20 times, leading to life-threatening muscle breakdown (rhabdomyolysis). There is no safe dose. If you’re on HIV meds, avoid simvastatin completely.
Is atorvastatin safe with HIV medications?
Yes, but only at low doses and only with certain HIV drugs. With darunavir/cobicistat, the maximum safe dose is 20 mg per day. With unboosted integrase inhibitors like dolutegravir or bictegravir, you can usually take up to 40-80 mg daily. Never exceed the recommended dose-higher amounts increase the risk of muscle damage.
What’s the safest statin for someone on HIV treatment?
Pitavastatin (Livalo) is generally the safest option. It’s metabolized through a different pathway and has minimal interaction with HIV drugs, including boosted regimens. Pravastatin is also low-risk and often used. Both are preferred over atorvastatin or rosuvastatin when possible, especially in older adults or those with kidney issues.
Do I need to stop my statin if I switch HIV meds?
Possibly. If you switch from a boosted regimen (like Prezcobix) to an unboosted one (like Biktarvy), your statin dose may need to be increased. If you switch from an unboosted regimen to a boosted one, your statin dose may need to be lowered. Always check for interactions before changing any medication. Never adjust your statin dose on your own.
Can I use over-the-counter statins or supplements like red yeast rice?
No. Red yeast rice contains a natural form of lovastatin and carries the same risks as prescription statins. It’s not safer-it’s unregulated and just as dangerous when combined with HIV drugs. Never use OTC cholesterol supplements without your doctor’s approval. They can interact just like prescription meds.
How often should I get blood tests if I’m on HIV meds and a statin?
Get a baseline test before starting the statin. Then repeat creatine kinase (CK) and liver function tests 4-6 weeks after starting or changing the dose. After that, annual checks are usually enough if you feel fine. But if you develop muscle pain, weakness, or dark urine, get tested immediately-don’t wait.
What should I do if I accidentally took a dangerous statin with my HIV meds?
Stop taking the statin immediately and contact your doctor or go to the nearest emergency room. Muscle damage can develop quickly. Symptoms like severe muscle pain, weakness, or dark urine require urgent evaluation. Blood tests for CK and kidney function are essential. Don’t wait to see if symptoms get worse.
Next Steps: What to Do Today
If you’re on HIV medication and taking-or thinking about taking-a statin, here’s what to do right now:- Find out exactly which HIV drugs you’re taking. Write down the full names (e.g., “darunavir/cobicistat” not just “my HIV pill”).
- Go to hiv-druginteractions.org and search for your combination. It’s free, updated monthly, and trusted by clinics worldwide.
- Call your doctor or pharmacist. Ask: “Is my statin safe with my HIV meds? What’s the maximum dose I can take?”
- If you’re not on a statin but have high cholesterol or heart risk factors, ask: “Should I be on one? Which one is safest for me?”
Heart health isn’t optional for people with HIV. But neither is safety. With the right information and the right tools, you can protect both your heart and your body.
Henry Sy
January 16, 2026 AT 04:01so i took simvastatin for like 3 days with my darunavir/cobicistat and thought i was just sore from the gym. turned out my CK was through the roof. ER visit, 2 days in the hospital, and now i’m on pitavastatin. don’t be me. just don’t.
Anna Hunger
January 17, 2026 AT 17:00It is imperative that individuals on antiretroviral therapy consult with their pharmacists prior to initiating statin therapy. The pharmacokinetic interactions between CYP3A4 inhibitors and statins are well-documented in peer-reviewed literature, and deviations from recommended dosing thresholds may result in life-threatening rhabdomyolysis. Adherence to clinical guidelines is non-negotiable.
Dylan Livingston
January 18, 2026 AT 03:13Oh wow, another ‘here’s how to not die’ guide from the medical industrial complex. Let me guess-next they’ll tell us not to breathe oxygen because it might oxidize our cells? I’ve been on boosted regimens for 12 years, took 80mg of atorvastatin, and my muscles still work fine. The FDA’s just scared of liability. Also, pitavastatin costs $600 a month. You really think I’m gonna pay that when my cousin in Mexico sells me generic simva for $5? 😌
says haze
January 19, 2026 AT 03:16It’s fascinating how medicine has become a series of algorithmic constraints rather than holistic care. We reduce complex human physiology to enzyme pathways and dosing caps, then call it ‘science.’ Meanwhile, the real issue-systemic neglect of cardiovascular prevention in marginalized populations-goes unaddressed. You can’t pharmacologically outmaneuver poverty, food deserts, and chronic stress with a 10mg tablet of rosuvastatin. The real interaction isn’t between ritonavir and CYP3A4-it’s between capitalism and survival.
Alvin Bregman
January 20, 2026 AT 13:37man i just found out my doc put me on lipitor without checking my hiv med and now im paranoid every time i lift weights. i think i might have rhabdo. or maybe im just tired. who knows anymore. anyway the hiv-druginteractions.org site is legit, saved my life
Sarah -Jane Vincent
January 20, 2026 AT 15:24EVERYONE KNOWS statins are just Big Pharma’s way of keeping you dependent. The real cause of heart disease in HIV patients? Chronic inflammation from government-mandated ART protocols. They don’t want you to know that niacin and turmeric fix everything. Also, the liver enzyme thing? Total lie. Your liver doesn’t care about CYP3A4-it cares about your soul. Stop trusting doctors. Start trusting your intuition. And for god’s sake, stop eating gluten.
Jason Yan
January 22, 2026 AT 05:51It’s wild how much we’ve changed. When I was first diagnosed in 2005, we were just happy to be alive. Now we’re worrying about whether our cholesterol meds will kill us before HIV does. I get that we’re living longer, but it feels like we’re trading one set of fears for another. I’ve been on Biktarvy and pravastatin for five years now-no issues. But I still check the Liverpool site every time I get a new prescription. Knowledge isn’t power here-it’s peace of mind.
shiv singh
January 23, 2026 AT 14:01you think this is bad? try being an immigrant with no insurance and your doctor tells you to take a $500 pill and you don’t even know what it does. my cousin took pitavastatin and got a bill for $12,000. they don’t care about us. they just want you to be quiet and take your pills. this whole thing is a scam. i’m switching to coconut oil and prayer.
Robert Way
January 23, 2026 AT 16:01so i asked my pharma if i could take fluvastatin with my atazanavir and they said maybe but dont go over 40mg but i think they misspelled something? like i think they meant 4mg? anyway i took 20mg and felt fine but now my pee is kinda brown?? should i be worried??
Sarah Triphahn
January 23, 2026 AT 20:04Everyone’s acting like this is new. It’s not. People have been dying from statin-HIV interactions since the 90s. But no one talks about it because the system doesn’t want you to know how fragile your life is. You think you’re safe because you’re ‘undetectable’? That’s a lie. Your body is a warzone. And statins? Just another weapon turned against you.
Vicky Zhang
January 25, 2026 AT 11:53I just want to say thank you to whoever wrote this. I’m 58, have been HIV+ since 2001, and just started pitavastatin last month. My heart feels lighter. My legs don’t ache anymore. I cried when I read the part about monitoring-my doctor never told me to check CK levels. I called her today and she adjusted everything. You’re not alone. You’re not broken. You just need the right info. And now you have it. ❤️