Taking five or more prescription medications is common for adults over 60. In fact, 41% of people aged 75 and older are on ten or more drugs daily. It’s not unusual-diabetes, high blood pressure, arthritis, cholesterol, and depression often come together. But the more pills you take, the higher the risk of dangerous mix-ups. Drug interactions can cause dizziness, kidney damage, internal bleeding, or even death. And many of these problems are preventable.
Why Multiple Prescriptions Are a Hidden Danger
You might think if each doctor prescribed your meds, they must be safe together. But that’s not how it works. Your cardiologist doesn’t see what your rheumatologist prescribed. Your primary care doctor might not know about the turmeric supplement you take for joint pain. And your pharmacist? They only see what you fill at their store. A 2022 study of over 15,000 Medicare patients found that people who used multiple pharmacies had a 58% higher risk of serious drug interactions. Why? Because no single provider has the full picture. One drug might raise your blood pressure. Another might lower it. Taken together, they cancel each other out-or worse, overload your liver or kidneys. The American Geriatrics Society lists 30 dangerous combinations to avoid in older adults. For example, mixing NSAIDs like ibuprofen with blood thinners can cause stomach bleeds. Taking calcium supplements at the same time as thyroid medicine blocks absorption. Even common OTC meds like antacids or sleep aids can interact with prescription drugs in ways you’d never guess.Step 1: Build a Complete Medication List
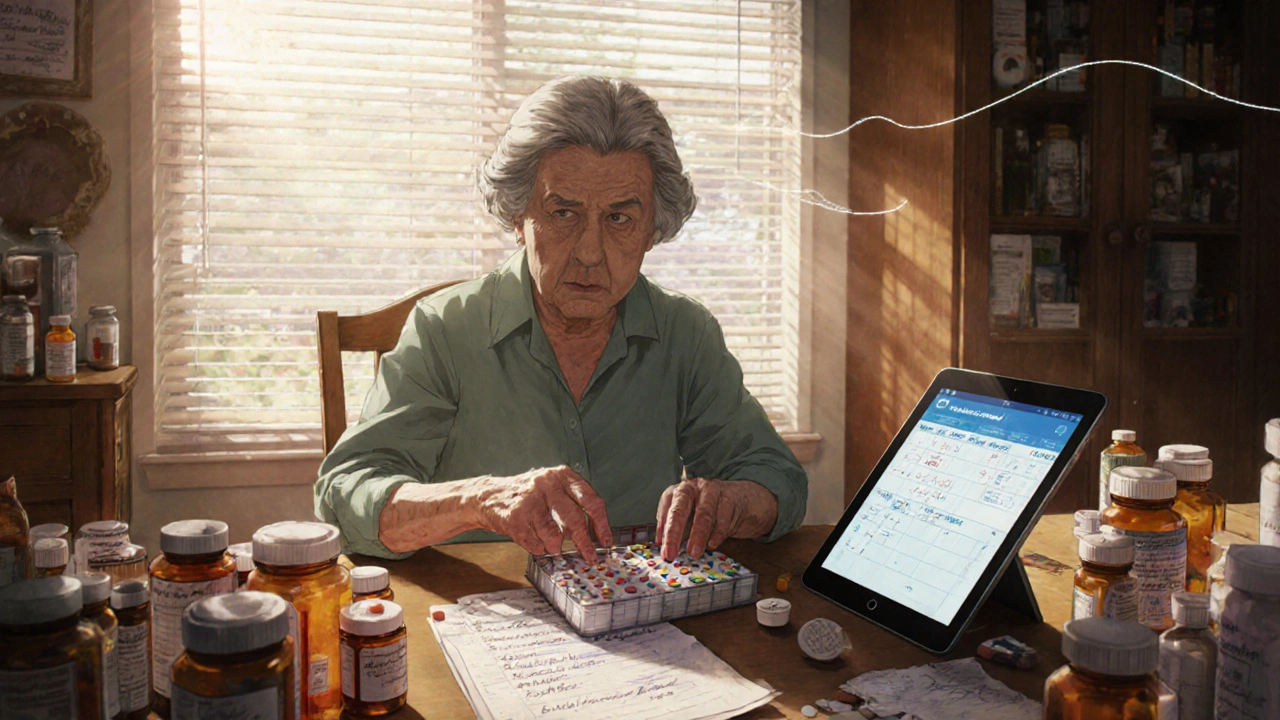
Start with every single thing you take-not just prescriptions. Include vitamins, herbal supplements, and over-the-counter pills. Many people forget these, but they’re often the hidden cause of problems. Ami Patel, a pharmacist and expert in medication safety, says 82% of dangerous interactions happen between prescriptions and supplements patients don’t mention. Your list needs details:- Drug name (brand and generic, e.g., “Lisinopril” or “Zestril”)
- Dosage (e.g., “10 mg”)
- When to take it (e.g., “every morning with breakfast”)
- Why you take it (e.g., “for high blood pressure”)
- Special instructions (e.g., “avoid grapefruit,” “take on empty stomach”)
Step 2: Use One Pharmacy for Everything
This is the single most effective step you can take. When you use the same pharmacy for all your prescriptions, they build a complete record of everything you’re taking. Pharmacists are trained to spot interactions you might miss. A 2023 Health Affairs study showed that single-pharmacy users had a 47% higher chance of catching dangerous drug combinations than those who split prescriptions across multiple stores. Why? Because pharmacists see your full history. They know you’re on warfarin and just got a new antibiotic. They’ll flag it before you even leave the counter. If you’re already using different pharmacies, switch. Call your new pharmacy and ask them to transfer all your prescriptions. Most will do it for free. You’ll get better advice, fewer errors, and a pharmacist who actually knows your meds.Step 3: Ask for Medication Synchronization
Medication synchronization (or “med sync”) is a free service offered by most community pharmacies. It means all your maintenance meds-those you take daily-are due for refill on the same day each month. Instead of going to the pharmacy four times a month, you go once. But here’s the real benefit: during med sync, pharmacists do a full medication review. They check for duplicates, outdated prescriptions, and interactions. The American Society of Health-System Pharmacists says properly run med sync programs reduce non-adherence by 31% and save $1,200-$1,800 per patient each year in avoided hospital visits. To join: ask your pharmacist if they offer med sync. If yes, they’ll set up an anchor date (like the first Friday of each month). They’ll adjust your refills so everything lines up. You might get a partial fill the first time to make it work. It takes 2-3 weeks to set up, but after that, it’s smooth sailing.
Step 4: Use a Pill Organizer
Even with perfect records, forgetting doses is common. A 2023 study in the Journal of General Internal Medicine tracked 1,245 older adults using 7-day pill organizers with morning and night compartments. Those who used them improved adherence from 62% to 87% in just six months. Simple plastic organizers cost under $15. Look for ones with alarms or timers. Devices like Hero Health’s smart dispenser cost around $899 and send alerts, lock doses, and notify family if a pill isn’t taken. But you don’t need tech to get results. Just fill your organizer every Sunday evening while watching your favorite show. Making it part of a routine increases success by 33%, according to the University of Michigan.Step 5: Talk to Your Doctor About Deprescribing
Not every pill you’ve been taking for years is still needed. Sometimes, meds lose their benefit over time-or become riskier as you age. The American Geriatrics Society, the American Society of Health-System Pharmacists, and the American Psychiatric Association all agree: regularly review your meds and deprescribe when appropriate. Ask your doctor: “Is this medicine still helping me? Could I stop one or two?” Don’t be afraid to bring your full medication list. Many doctors don’t realize how many pills their patients are taking. A 2023 study found that 68% of physicians use electronic systems that flag drug interactions-but those systems give false alarms 43% of the time. That means real dangers sometimes slip through. If your doctor says yes, stop a med, do it slowly. Never quit cold turkey unless told to. Some drugs need to be tapered to avoid withdrawal or rebound effects.Watch Out for These Common Dangerous Mixes
Here are a few high-risk combinations you should ask your pharmacist about:- NSAIDs + Blood Thinners (e.g., ibuprofen + warfarin): High risk of stomach bleeding.
- Calcium + Thyroid Meds: Calcium blocks absorption. Take them at least 2 hours apart.
- Statin + Grapefruit: Grapefruit juice can cause statins to build up to toxic levels in your blood.
- SSRIs + NSAIDs: Can increase bleeding risk, especially in older adults.
- Proton Pump Inhibitors (PPIs) + Magnesium Supplements: Long-term PPI use can lower magnesium. Don’t take magnesium without checking with your doctor first.
Digital Tools Can Help-But They’re Not for Everyone
Apps like Medisafe and MyMeds send reminders and track doses. A 2022 JAMA Internal Medicine trial showed they improved adherence by 28% compared to paper logs. But here’s the catch: 62% of adults over 75 don’t use smartphones regularly. If you’re not comfortable with tech, don’t force it. A paper list and a pill box work better than an app you never open. Some pharmacies like CVS offer free apps that send refill reminders 72 hours before you run out. That’s helpful-but only if you use your phone regularly. For many seniors, a simple phone call to the pharmacy is easier and just as effective.What to Do If You Feel Off
New dizziness? Unusual fatigue? Upset stomach? Dry mouth? These aren’t just “getting older.” They could be signs of a drug interaction. If you feel different after starting a new med or changing a dose, call your pharmacist first. They’re trained to spot these clues. Don’t wait for your next doctor’s appointment. A quick call can prevent a trip to the ER.The Big Picture: Why This Matters
Medication errors cost the U.S. healthcare system over $300 billion a year. One in five hospital admissions for people over 65 is due to a bad drug reaction. And the number of older adults taking multiple prescriptions is growing fast. But here’s the good news: coordinating your meds doesn’t require a miracle. It just needs a few simple, consistent habits. One pharmacy. A written list. A pill box. A monthly review. A willingness to ask questions. The result? Fewer hospital visits. More energy. Better sleep. Less fear. You’re not just managing pills-you’re taking back control of your health.What should I do if I’m taking more than five medications?
Start by gathering a full list of everything you take-including vitamins and supplements. Then, schedule a medication review with your pharmacist. Ask if you qualify for a medication synchronization program. These services help streamline refills and catch dangerous interactions. Also, talk to your doctor about whether any meds can be safely stopped or replaced.
Can I use different pharmacies for different prescriptions?
You can, but it’s risky. When prescriptions are split across multiple pharmacies, no single provider has your full medication history. This makes it harder to catch dangerous interactions. A 2023 study found patients using multiple pharmacies had a 58% higher risk of serious drug reactions. For safety, choose one pharmacy and transfer all your prescriptions there.
How often should I review my medications?
At least once every six months, or whenever you see a new doctor or start a new medication. Many pharmacies offer free medication therapy management (MTM) sessions-these are perfect for reviews. During these 20-30 minute appointments, pharmacists check for duplicates, side effects, and unnecessary drugs. Don’t wait for a problem to arise-be proactive.
Are over-the-counter supplements safe with my prescriptions?
Not always. Many people assume supplements are harmless, but that’s not true. St. John’s Wort can reduce the effectiveness of blood thinners and antidepressants. Garlic and ginkgo can increase bleeding risk. Even vitamin K can interfere with warfarin. Always tell your pharmacist and doctor about every supplement you take-even if you think it’s “natural.”
What’s the best way to remember when to take my pills?
Use a pill organizer with morning and night compartments, and fill it weekly on the same day-like Sunday evening. Pair it with a daily routine, like watching your favorite TV show. Set phone alarms if you’re comfortable with tech. If not, ask a family member to help remind you. The key is consistency. Missing doses increases the risk of complications and hospitalization.
Aidan McCord-Amasis
November 16, 2025 AT 03:24ASHISH TURAN
November 16, 2025 AT 08:40Ogonna Igbo
November 17, 2025 AT 16:35Adam Dille
November 18, 2025 AT 14:54Katie Baker
November 20, 2025 AT 03:08BABA SABKA
November 20, 2025 AT 13:18Jonathan Dobey
November 21, 2025 AT 13:06Hollis Hollywood
November 23, 2025 AT 09:09Ryan Airey
November 24, 2025 AT 04:35Chris Bryan
November 24, 2025 AT 12:41Shyamal Spadoni
November 25, 2025 AT 06:31John Foster
November 25, 2025 AT 21:25