When your doctor or pharmacist gives you advice about your medications, it’s easy to think, “I’ll remember this.” But by the time you get home, juggling kids, work, or just plain fatigue, details blur. Did they say take it with food or on an empty stomach? What side effect means you should call back? Was the refill number two or three? Writing it down isn’t just helpful-it’s essential. Proper documentation of provider advice about medications protects your health, prevents errors, and ensures everyone who treats you later has the full picture.
Why Documentation Matters More Than You Think
Medication errors cause about 7,000 deaths in the U.S. every year, according to the Institute of Medicine. A large chunk of those happen because someone didn’t have the right information. Maybe a pharmacist didn’t know you were allergic to a drug. Maybe a nurse gave you the wrong dose because the instructions weren’t clear. Or maybe you forgot what your doctor told you about timing or food restrictions. Good documentation fixes that. It turns spoken advice into a permanent, clear record. The American Medical Association, the Joint Commission, and the Centers for Medicare & Medicaid Services all require it. They don’t just suggest it-they enforce it. And it’s not just for doctors. Pharmacists, nurses, dentists, and even telehealth providers must document what they tell you. Your record isn’t just a note. It’s a legal document. If something goes wrong, that paper-or digital file-could be read aloud in court. That’s why every entry must be dated, signed or initialed, and specific. Vague statements like “patient advised” won’t cut it. You need details.What Exactly to Write Down
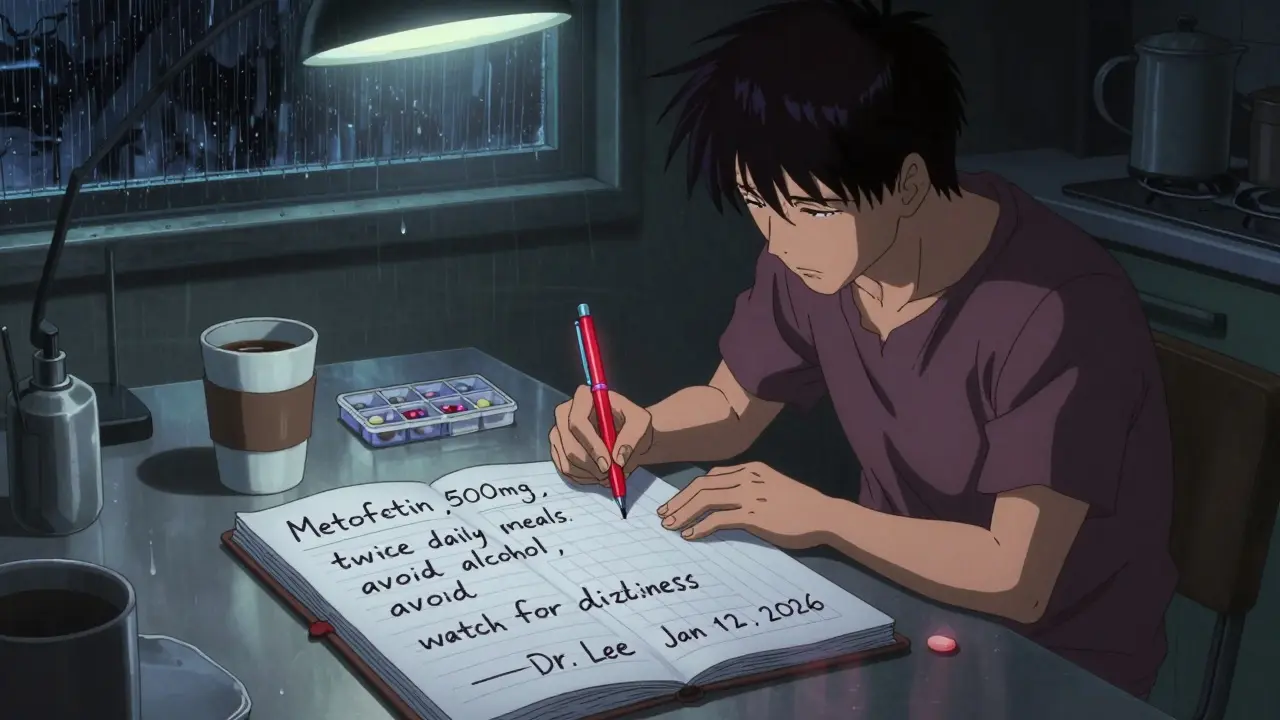
Don’t just scribble “take pill.” Here’s what you need to capture:- Medication name: Brand and generic if different. Don’t say “the blue pill.” Write “metformin 500 mg” or “Lipitor 20 mg.”
- Dose and frequency: “Take one tablet by mouth twice daily with breakfast and dinner.” Not “take twice a day.”
- Duration: “For 14 days” or “until finished.” If it’s long-term, note that too.
- Refills: How many are allowed? And when can you refill?
- Special instructions: “Take on empty stomach,” “avoid alcohol,” “shake well before use,” “do not crush.”
- Side effects to watch for: “If you feel dizzy or have a rash, call immediately.”
- Allergies and reactions: “Allergic to penicillin-rash and swelling.” Don’t assume they know. Write it down.
- What was discussed: “Explained risk of bleeding with warfarin. Patient understood and agreed to weekly INR checks.”
How to Record It-Paper or Digital?
You can use a notebook, a phone app, or your provider’s patient portal. But whichever you choose, follow these rules:- Date and time every entry. Even if you write it right after the visit, note when.
- Write clearly. If you’re handwriting, use block letters. If typing, avoid autocorrect errors.
- Use the same format every time. Consistency helps you and future providers scan quickly.
- Include who gave the advice. “Dr. Lee, Jan 12, 2026” or “Pharmacist Patel, Jan 13, 2026.”
What to Do When You Don’t Understand
If something doesn’t make sense, don’t nod and smile. Say, “Can you write that down for me?” Or, “Can you explain it again? I want to make sure I get it right.” Ask for clarification on:- Why you’re taking this medication.
- What happens if you skip a dose.
- What to do if you feel worse.
- Whether it interacts with anything else you take-vitamins, supplements, even over-the-counter painkillers.
What to Do If You Refuse or Skip a Medication
Sometimes, you decide not to take a drug. Maybe it’s too expensive. Maybe you’re scared of side effects. Maybe you just don’t think it’s helping. Whatever the reason, document it. Write: “Patient declined metoprolol due to concern about fatigue. Discussed alternatives. Will re-evaluate in 2 weeks.” This isn’t about blaming you. It’s about protecting your care. If you later end up in the ER with high blood pressure, and they see you were prescribed a beta-blocker but never took it, they’ll know why. Without that note, they might assume you didn’t get it-or worse, that you’re noncompliant. The National Committee for Quality Assurance found that poor documentation of refusals contributes to 22% of preventable drug-related hospital visits.How to Share This With Other Providers
You might see a specialist, visit an urgent care center, or go to the ER. They won’t have your full history unless you bring it. Carry a printed copy of your medication list and provider advice. Or use a free app like MyMedList or Medisafe to store it digitally. When you go in, say: “Here’s what my doctor told me about my meds.” Hand it over. Don’t assume they’ll check your records. Not all systems talk to each other. Even if they do, they might not have the full context of your conversation.
What Happens If You Don’t Document It
Skipping documentation isn’t just risky-it’s dangerous. - A 2022 study found that 38% of medical malpractice claims involving medications were due to poor documentation. - CMS can deny payment if your medical record doesn’t clearly show what was prescribed and why. - In dental care, failing to document a conversation about a painkiller prescription can lead to legal liability. - If you switch providers, your new doctor might prescribe something that interacts with a drug you’re already taking-because they never knew you were on it. The bottom line: If it wasn’t written down, it didn’t happen-legally and medically.What’s Changing in 2025
By 2025, nearly all medication documentation will happen through connected electronic systems. The FDA is pushing a new rule: every prescription will come with a standardized, one-page patient fact sheet-like a nutrition label for drugs. It’ll list key info: purpose, dosage, warnings, side effects, storage. You’ll get this digitally or printed. But even with this, your personal notes still matter. The fact sheet won’t tell you what your provider said about your specific situation-like “take it before bed because it makes you drowsy,” or “avoid grapefruit because it messes with absorption.” Also, starting in 2024, Medicare requires doctors to document current medications at every visit. If they don’t, they lose money. That means more attention to this step-but only if you remind them to be thorough.Final Checklist: Your Medication Documentation Kit
After every visit, run through this:- Did I write down the full name of each medication?
- Did I note the exact dose and how often to take it?
- Did I record special instructions (food, timing, warnings)?
- Did I write down the number of refills?
- Did I list any side effects I was told to watch for?
- Did I note any allergies or past reactions?
- Did I record who gave the advice and when?
- Did I write down if I refused or skipped a medication?
- Did I update my digital or paper copy?
- Did I share this with my pharmacist or next provider?
Good documentation isn’t extra work. It’s your safety net. It turns confusion into clarity. It turns guesswork into confidence. And in healthcare, that’s not just helpful-it’s life-saving.
What if I can’t remember what my provider said about my meds?
Call the provider’s office. Most have a nurse or pharmacist who can review your visit summary. Ask them to email or mail you a written summary. If you’re using a patient portal, check for a visit note. If it’s missing, send a secure message asking for clarification. Don’t rely on memory-especially with complex regimens.
Do I need to document advice from a pharmacist too?
Yes. Pharmacists are medication experts. If they explain how to use a new drug, warn about interactions, or suggest a cheaper alternative, write it down. Their advice is part of your care plan. The American Society of Health-System Pharmacists requires this documentation. It protects you and ensures other providers know you received counseling.
Can I use my phone to record provider conversations?
Legally, you can record conversations in most places if you’re part of them. But it’s not ideal. Recordings are hard to search, take time to review, and may not be accepted in legal or medical reviews. Writing a clear, concise note is faster, more reliable, and easier to share. If you do record, always transcribe the key points into written form immediately after.
How long should I keep medication documentation?
Keep your personal records for at least 10 years, or longer if you have chronic conditions. Medical providers are required to keep records for 7-10 years, depending on state law. But your own copy is your backup. If you move, change doctors, or need care years later, having your own history saves time and prevents dangerous gaps.
What if my provider refuses to document advice?
Politely insist. Say, “I want to make sure I follow your advice correctly. Could you please write this down or add it to my chart?” If they still refuse, ask to speak to the office manager. You have a right to accurate records under federal law. If the issue continues, consider switching providers. Poor documentation is a red flag for overall care quality.
Nicholas Miter
January 26, 2026 AT 12:07Been doing this for years after my grandma had that mix-up with blood thinners. Just keep a little notebook in your wallet. Write it down like you’re texting your bestie-no fancy stuff. 'Take metformin w/ breakfast, no alcohol, dizziness = call doc.' Done. Saved my ass more than once.
Also, if you use a phone app, make sure it syncs. I lost a whole month of notes when my phone died and iCloud forgot to back it up. Lesson learned.
TONY ADAMS
January 26, 2026 AT 22:53why tf do i have to write all this down? my doctor knows my history. they’ve been my doc for 12 years. this is just bureaucratic nonsense. i trust them. why are we turning healthcare into a paperwork nightmare?
Ashley Karanja
January 28, 2026 AT 12:22As someone who’s navigated the labyrinth of polypharmacy with chronic autoimmune issues, I can’t stress enough how vital this is-not just for safety, but for psychological peace of mind. When you’re drowning in meds, the cognitive load is real. Documenting isn’t just clinical-it’s an act of self-advocacy rooted in neurodivergent and disability justice frameworks. Writing it down externalizes the burden from your hippocampus to a tangible, retrievable artifact. And when you’re in crisis mode, that artifact becomes your anchor.
Also, I use Notion with color-coded tags: 🟡 for new prescriptions, 🔴 for contraindications, 🟢 for refills. It’s not just data-it’s a relational ledger between me and my body. Emoji aren’t frivolous; they’re cognitive scaffolding. 🙏
Curtis Younker
January 29, 2026 AT 18:19THIS. This right here is the kind of stuff that actually saves lives. I used to think I was too busy to write stuff down-until my mom ended up in the ER because she forgot which pill she was supposed to take twice a day. Turned out she’d been taking the wrong one for three weeks.
Now I have a little whiteboard in my kitchen with everyone’s meds. My 80-year-old dad even uses it. He says it’s like having a nurse living in his pantry. Seriously, if you’re not doing this, you’re playing Russian roulette with your health. Just do it. Your future self will thank you.
Also, use the damn patient portal. It’s free. It’s right there. Stop making it harder than it is.
Ryan W
January 30, 2026 AT 11:56Let’s be real: this entire framework is built on the assumption that patients are literate, technologically literate, and have access to consistent healthcare infrastructure. What about rural patients without broadband? Elderly folks who can’t read small print? Non-native English speakers? This isn’t ‘self-care’-it’s a neoliberal burden dumped onto vulnerable populations under the guise of ‘empowerment.’
And don’t get me started on the FDA’s ‘nutrition label’ for drugs. That’s marketing, not medicine. If you think a one-pager explains warfarin’s interaction with kale, you’ve never met a real pharmacist.
Systemic change is needed. Not more paperwork for patients.
Henry Jenkins
January 31, 2026 AT 23:46Interesting perspective. I’ve been thinking about this differently since my sister had her stroke last year. The ER docs had zero access to her meds because she never documented them-she thought her primary care doctor had it all on file. Turns out, he didn’t update it in two years.
So now I’m trying to figure out the balance: how much responsibility should fall on the patient vs. the system? I get that documentation is critical, but why is it so damn hard to get a simple, standardized, interoperable record across providers? Why does every hospital have its own portal with its own login and its own format?
Maybe the real issue isn’t that patients aren’t documenting enough-it’s that the system refuses to make documentation easy. We’re asking people to fix a broken system with sticky notes and apps. That’s not empowerment. That’s exhaustion by design.
Ashley Porter
February 2, 2026 AT 12:26Just a quick note: if you're using a patient portal, always check the 'Medications' tab after your visit. I once thought my doc added a new antibiotic, but it was just a draft. Took me three days to realize I never actually got the script. The portal doesn't auto-publish. You have to verify. Don't assume. Always verify.
George Rahn
February 3, 2026 AT 08:50It is not merely prudent, nor is it simply prudent-it is a civic and moral imperative, a solemn obligation incumbent upon every citizen of this republic to safeguard the sanctity of the therapeutic contract. The erosion of accurate, legible, and contemporaneous documentation is not a mere administrative oversight; it is the slow, insidious decay of the Hippocratic covenant itself. In an age where the commodification of care has reduced the physician-patient relationship to a transactional exchange, the written word becomes the last bulwark against the tyranny of forgetfulness, the chaos of miscommunication, and the arrogance of institutional negligence.
Let us not forget: the ink of a well-documented prescription is more potent than the most expensive pharmaceutical. It is the echo of wisdom, the crystallization of intent, the immutable testament to human dignity in the face of biological fragility. To neglect it is not negligence-it is sacrilege.
And to those who dismiss this as 'busywork'-I say: when your child is given the wrong dose because a nurse couldn’t decipher a scribbled note, will you still call it 'busywork'? I think not.