Hypertension Drug Selection Tool
Find the Best Hypertension Medication for You
This tool helps you compare different hypertension medications based on your health conditions and preferences. Select your criteria to see which options might work best for you.
Recommended Options
Select your criteria and click 'Find Your Best Option' to see recommendations.
If you’re scanning pharmacy shelves for a blood‑pressure pill, you’ve probably seen the name Avalide. It’s a combo of irbesartan and hydrochlorothiazide that promises to lower blood pressure in one go. But is it really the best fit for you, or are there other options that might work better?
Key Takeaways
- Avalide mixes an ARB (irbesartan) with a thiazide diuretic, targeting two mechanisms at once.
- Pure ARBs like losartan or valsartan avoid the diuretic side‑effects but may need a separate thiazide.
- ACE inhibitors (e.g., lisinopril) work differently and can cause cough, which most ARBs don’t.
- Cost, kidney function, and electrolyte balance are the main factors when choosing an alternative.
- Always discuss any switch with a doctor, especially if you have diabetes or chronic kidney disease.
What is Avalide?
Avalide is a fixed‑dose combination tablet that contains irbesartan 150mg, 300mg, or 450mg, paired with hydrochlorothiazide 12.5mg or 25mg. It belongs to the angiotensinII receptor blocker (ARB) class, while the diuretic component belongs to the thiazide family. Approved in Australia in 2008, Avalide is prescribed for adults with primary hypertension who need a two‑pronged approach to bring their systolic readings below 140mmHg.
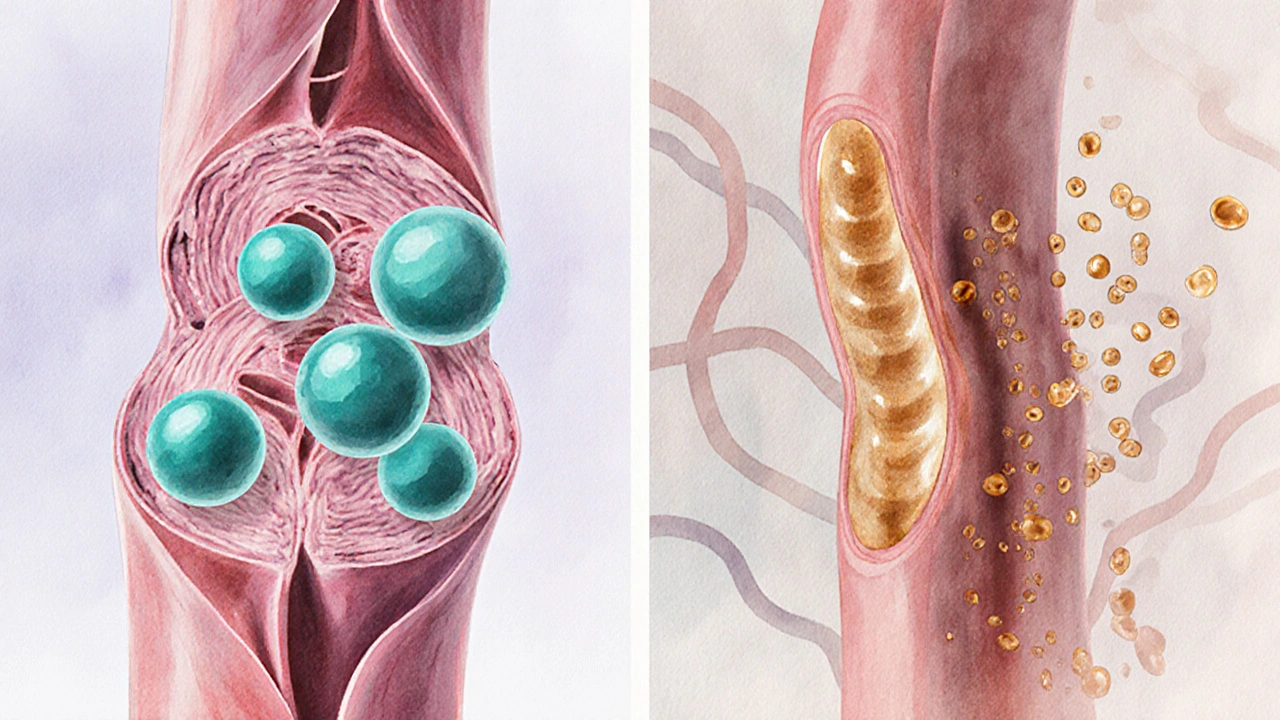
How Avalide Works
- Irbesartan blocks the angiotensinII receptor, preventing vasoconstriction and reducing aldosterone‑driven sodium retention.
- Hydrochlorothiazide increases urine output, flushing excess salt and water, which further lowers blood volume.
- The combo cuts both vascular resistance and fluid overload, often achieving a 10‑15mmHg drop in systolic pressure within weeks.
Alternatives to Avalide
When doctors consider swapping or starting a different regimen, they usually look at three groups: pure ARBs, ACE inhibitors, and other thiazide‑based combos.
| Drug (Brand) | Class | Typical Dose Range | Key Benefits | Main Drawbacks | Average Cost (AU$) per month |
|---|---|---|---|---|---|
| Avalide | ARB + Thiazide | Irbesartan 150‑450mg + HCTZ 12.5‑25mg | Two‑in‑one convenience; strong BP drop | Risk of electrolyte loss; may aggravate gout | ≈ $45‑$60 |
| Cozaar (Losartan) | ARB | 25‑100mg daily | Well‑tolerated; low cough risk | Often needs added diuretic for full control | ≈ $30‑$45 |
| Diovan (Valsartan) | ARB | 80‑320mg daily | Proven cardiovascular protection | May cause dizziness at high doses | ≈ $35‑$50 |
| Benicar (Olmesartan) | ARB | 20‑40mg daily | Effective in resistant hypertension | Rare risk of sprue‑like enteropathy | ≈ $40‑$55 |
| Prinivil (Lisinopril) | ACE Inhibitor | 5‑40mg daily | Renal protection in diabetics | Cough and angio‑edema possible | ≈ $20‑$35 |
| Enalapril | ACE Inhibitor | 5‑20mg twice daily | Good for heart failure patients | Same cough risk; needs twice‑daily dosing | ≈ $25‑$40 |
| Hydrodiuril (Hydrochlorothiazide alone) | Thiazide Diuretic | 12.5‑25mg daily | Low cost; easy combo with any ARB/ACE | Electrolyte disturbances if not monitored | ≈ $5‑$10 |
Deep Dive into Each Alternative
Losartan (Cozaar)
Losartan is an ARB that blocks the same receptor as irbesartan but with a slightly weaker affinity. It’s a go‑to when patients can’t tolerate a diuretic. Studies in Australian cohorts show an average 10mmHg systolic reduction when paired with a thiazide, comparable to Avalide’s single‑pill effect.
Valsartan (Diovan)
Valsartan offers robust blood‑pressure control and has solid evidence for reducing heart‑failure hospitalizations. It’s often chosen for patients with a history of myocardial infarction because of its proven cardioprotective data.
Olmesartan (Benicar)
Olmesartan is a newer ARB with high receptor selectivity. It shines in resistant hypertension but carries a rare gut‑related side‑effect (sprue‑like enteropathy) that doctors watch for.
Lisinopril (Prinivil)
Lisinopril belongs to the ACE inhibitor family. By blocking the conversion of angiotensinI to II, it reduces both pressure and proteinuria. The main trade‑off is a persistent dry cough in up to 10% of users.
Enalapril
Enalapril works the same way as lisinopril but often requires twice‑daily dosing. It’s a solid choice for heart‑failure patients, though the cough risk remains.
Hydrochlorothiazide (solo)
Hydrochlorothiazide alone is cheap and effective, but on its own it may not achieve target BP in moderate‑to‑severe hypertension. Doctors usually add an ARB or ACE inhibitor to cover the vascular component.

Choosing the Right Regimen
Deciding between Avalide and a separate‑pill strategy hinges on three practical questions:
- Do you need a diuretic? If you have fluid retention, edema, or a history of heart failure, the built‑in thiazide is a win.
- Are electrolyte issues a concern? The combo raises the chance of low potassium or high uric acid. Patients with gout or kidney stones often prefer a pure ARB plus a low‑dose diuretic prescribed separately.
- What’s your budget? Avalide’s convenience costs a bit more than a generic ARB + generic thiazide bought separately. However, for patients on government subsidies, the price gap narrows.
Another subtle factor is adherence. One pill a day beats two for many people, especially older adults who juggle multiple medicines.
Safety, Side Effects, and Monitoring
All the drugs listed share a core set of possible adverse events-dizziness, low blood pressure, and kidney function changes. Specific nuances include:
- Electrolyte loss: More common with Avalide and solo hydrochlorothiazide; monitor potassium and sodium.
- Cough: Predominantly an ACE inhibitor issue; switches to an ARB usually resolve it.
- Angio‑edema: Rare but serious; can happen with any ARB or ACE inhibitor.
- Gout flare: Thiazides raise uric acid, so patients with a gout history may need a non‑diuretic ARB alone.
Baseline labs (creatinine, eGFR, electrolytes) before starting, then repeat after 2‑4 weeks, are standard practice in Australian clinics. Pregnant women should avoid all ARBs and ACE inhibitors; alternatives like methyldopa are used instead.
Frequently Asked Questions
Can I switch from Avalide to a single ARB without a diuretic?
Yes, many doctors start patients on a pure ARB like losartan and add a low‑dose thiazide only if blood pressure stays high. This approach lets you tailor the diuretic dose and reduces electrolyte‑related side‑effects.
Is Avalide safe for people with chronic kidney disease?
It can be used, but kidney function must be closely monitored. The ARB part protects the kidneys, while the thiazide can worsen low‑potassium levels, so dose adjustments are often needed.
Why does my doctor prescribe a combo pill instead of two separate tablets?
Convenience and adherence are the main reasons. One pill reduces the chance of missed doses, especially in older patients who may be on five or more medicines.
What should I do if I develop a persistent cough on lisinopril?
Contact your prescriber. Most clinicians will switch you to an ARB like irbesartan or losartan, which usually stops the cough within a couple of weeks.
Are there any dietary restrictions while taking a thiazide diuretic?
Limit high‑salt foods to avoid counteracting the diuretic’s effect. Also, ensure adequate potassium intake (bananas, yoghurt) unless your doctor advises a supplement.
Bottom line: Avalide delivers a handy, two‑in‑one solution, but it isn’t a one‑size‑fits‑all. Pure ARBs, ACE inhibitors, or separate thiazide combos can offer cheaper, more flexible options, especially if you have specific side‑effect concerns or kidney‑function considerations. Talk to your GP or cardiologist, run the necessary labs, and pick the regimen that keeps your pressure down without creating new problems.

Chris Atchot
October 13, 2025 AT 12:32When you start Avalide, the first thing to remember is that you are taking two active agents in one tablet! Irbesartan works by blocking the angiotensin‑II receptor, which relaxes your blood vessels and reduces the workload on the heart. Hydrochlorothiazide, the companion thiazide, increases urine output, helping to shed excess sodium and water. Because the diuretic part can push potassium out of your cells, you should have your serum potassium checked within the first two weeks of therapy. A drop below 3.5 mmol/L may cause muscle cramps, fatigue, or even arrhythmias, so supplementation or dietary adjustments might be necessary. If you have a history of gout, be aware that thiazides can raise uric acid levels, potentially triggering a flare. In such cases, your doctor might prefer a pure ARB like losartan and add a low‑dose thiazide separately, or prescribe allopurinol prophylactically. Renal function is another key factor; the ARB component protects the kidneys, but the thiazide can reduce glomerular filtration if you are already low on eGFR. Therefore, a baseline creatinine and eGFR should be obtained before starting, followed by another check after one month. Patients on concurrent potassium‑sparing diuretics, such as spironolactone, need extra caution, as the combination may lead to hyperkalemia. If you experience dizziness or light‑headedness, especially when standing up quickly, it could be a sign of volume depletion from the thiazide. Hydration is important, but avoid excessive salt intake, which can blunt the effect of the diuretic. Cost‑wise, the single‑pill combo often seems pricier than separate generics, but insurance subsidies can narrow that gap considerably. Adherence improves dramatically when you only have to remember one pill a day, a fact supported by numerous compliance studies. Lastly, never stop Avalide abruptly without consulting your prescriber; a gradual taper may be needed to avoid rebound hypertension. Keeping a simple medication journal can help you and your healthcare team spot trends and adjust the regimen safely!
Sönke Peters
October 25, 2025 AT 20:32Sticking to one pill a day really helps keep the routine simple.
Todd Anderson
November 7, 2025 AT 03:32Combination therapy embodies a dialectic between simplicity and specificity, wherein a single pill attempts to reconcile multiple physiological pathways. The ARB component attenuates the renin‑angiotensin system, while the thiazide addresses volume overload. From a mechanistic standpoint, this duality can be advantageous, yet it also obliges the clinician to consider additive adverse effect profiles. Moreover, the ethical imperative to individualize therapy remains paramount, despite the allure of convenience. Consequently, the decision to employ Avalide should arise from a balanced deliberation of evidence and patient context.
Dexter Smith
November 19, 2025 AT 11:32From a cost perspective, Avalide often sits at the top of the price ladder, especially when compared to generic losartan plus a cheap thiazide. The premium you pay for the convenience of a single tablet may not justify the marginal blood‑pressure gain. Moreover, the fixed dose limits your ability to fine‑tune each component, which can lead to suboptimal electrolyte balance. In practice, many clinicians find that splitting the agents yields both financial and clinical flexibility.
Cherish Capps
December 1, 2025 AT 19:32Hey fam, if ur thinking about switchin to Avalide, just remember to keep an eye on ur potassium levels, ok? The combo can knock ur potassium down quite a bit, so a banana a day or a mild supplement can help. Also, if u got gout, the thiazide part might make it worse, so talk to ur doc about alternatives. Stay chill and keep that blood pressure in check!
Amy Carpenetti
December 14, 2025 AT 03:32Cost is a factor but insurance can cover a lot of it. Some patients get the combo for free. It also reduces pill burden which matters. Ultimately consider overall health goals.
Paul Griffin
December 26, 2025 AT 11:32Monitoring laboratory parameters is essential when initiating Avalide. Baseline serum potassium, creatinine, and eGFR should be obtained before the first dose. Re‑check these values after two weeks, and again at one month, to ensure stability. If abnormalities arise, dosage adjustment or component separation may be indicated. Consistent follow‑up appointments will help maintain therapeutic success.
Michael Tekely
January 7, 2026 AT 19:32When you titrate the irbesartan‑hydrochlorothiazide combo, think of pharmacodynamics versus pharmacokinetics. Start at the lowest strength, observe the antihypertensive response, then adjust based on home BP logs. If you notice orthostatic symptoms, consider a slower uptitration schedule. The diuretic’s natriuretic effect can be modulated by dietary sodium intake, so counsel patients accordingly. This iterative approach maximizes efficacy while minimizing electrolyte perturbations.
Oscar Taveras
January 20, 2026 AT 03:32Indeed, the elegance of a fixed‑dose combination lies in its ability to streamline therapy while preserving efficacy. Patients often report higher satisfaction when their regimen is simple, which can translate into better long‑term outcomes. Embracing such innovations, when appropriate, reflects a progressive stance in modern hypertension management 😊. Nonetheless, clinical judgment must always guide the final decision.
katie clark
February 1, 2026 AT 11:32One must recognize that the discourse surrounding fixed‑dose regimens frequently suffers from a paucity of nuanced pharmacological insight. The superficial allure of convenience belies the intricate interplay of receptor dynamics and renal handling. A discerning practitioner ought to prioritize individualized titration over mere simplification.