Steroid Hyperglycemia Insulin Calculator
How to Use This Tool
Enter your current steroid dose and insulin regimen to calculate recommended adjustments. Based on clinical guidelines for steroid-induced hyperglycemia.
Recommended Adjustments
Basal Insulin Adjustment
Adjust to:
Mealtime Insulin Adjustment
Adjust to:
What Is Steroid Hyperglycemia?
Steroid hyperglycemia happens when steroids-like prednisone, hydrocortisone, or dexamethasone-cause blood sugar to spike. It’s not just a side effect. It’s a direct metabolic disruption. Even people without diabetes can develop high blood sugar after starting steroids. For those already living with type 1 or type 2 diabetes, it can turn a manageable condition into a dangerous one.
This isn’t rare. About 40% of hospital endocrinology consults are for patients whose blood sugar went out of control after starting steroids. In some cases, over 80% of patients on high-dose steroids have at least one episode of high blood sugar. The problem? Most of it happens after meals, not when fasting. That means checking your sugar only in the morning misses half the picture.
Why Do Steroids Raise Blood Sugar?
Steroids don’t just make you hungry. They mess with how your body uses insulin. Here’s how:
- They block insulin action: Steroids interfere with the signals that tell your muscles and fat cells to take in glucose. Your cells become resistant, so sugar stays in your blood.
- They tell your liver to make more sugar: Your liver starts pumping out glucose like it’s in emergency mode-even when you don’t need it.
- They quiet your pancreas: Beta cells in your pancreas produce less insulin when steroids are around. In some cases, they stop working entirely for a while.
- They boost stress hormones: Glucagon, epinephrine, and cortisol all rise, which further pushes glucose into your bloodstream.
This isn’t just about eating too much. It’s about your body being forced into a state of metabolic chaos. That’s why sliding scale insulin alone often fails. You need a plan that matches the steroid’s timing, not just your blood sugar readings.
Who’s at Highest Risk?
Not everyone on steroids gets hyperglycemia. But some people are far more likely to. Here’s who needs the most attention:
- People with existing diabetes: Especially type 2. Their insulin resistance is already high. Steroids push it over the edge.
- Those on high doses: A daily dose of 20 mg prednisone or higher doubles the risk. At 100 mg, the chance of needing insulin jumps fivefold.
- Older adults: Age 65 and up. Their pancreas doesn’t bounce back as easily.
- People with obesity: BMI over 30? You’re already insulin resistant. Steroids make it worse.
- Those on other immunosuppressants: Tacrolimus (used after transplants) cuts insulin production by 35-45%. Combine that with steroids, and blood sugar can skyrocket.
- People with low magnesium: Every 0.1 mg/dL drop in magnesium raises hyperglycemia risk by 10-15%.
And here’s something many miss: if you’ve had gestational diabetes, you’re at higher risk-even if your sugar returned to normal. Steroids can wake that old problem back up.
How to Adjust Insulin for Steroid-Induced Hyperglycemia
You can’t treat steroid hyperglycemia like regular diabetes. The timing matters as much as the dose.
Basal insulin: Increase by 20-30% when starting moderate to high-dose steroids. For example, if you were on 20 units of long-acting insulin daily, bump it to 24-26 units. This helps control the constant glucose production from your liver.
Mealtime insulin: This is where most people fail. Steroids cause the biggest spikes 4-8 hours after taking them. If you take steroids in the morning, your breakfast and lunch will be hardest to control. You may need to increase your rapid-acting insulin by 50-100% for those meals. Dinner? Often unchanged.
Example: A patient on 10 mg prednisone daily takes it at 8 a.m. Their blood sugar is 120 mg/dL before breakfast. Normally, they’d take 6 units of insulin. Now, they may need 9-12 units. Same for lunch. But by dinner, their sugar might be fine without extra insulin.
For patients on dexamethasone (a long-acting steroid), the spike lasts longer. Insulin adjustments need to cover more hours. For hydrocortisone (short-acting), you might need to adjust insulin twice a day.
Monitoring: What to Check and When
Don’t rely on fasting glucose. That’s like checking your car’s oil only when you’re parked. You need to see what’s happening while you’re driving.
Recommended checks:
- Before breakfast
- 2 hours after breakfast
- Before lunch
- 2 hours after lunch
- Before dinner
- 2 hours after dinner
- At bedtime
- Any time you feel off
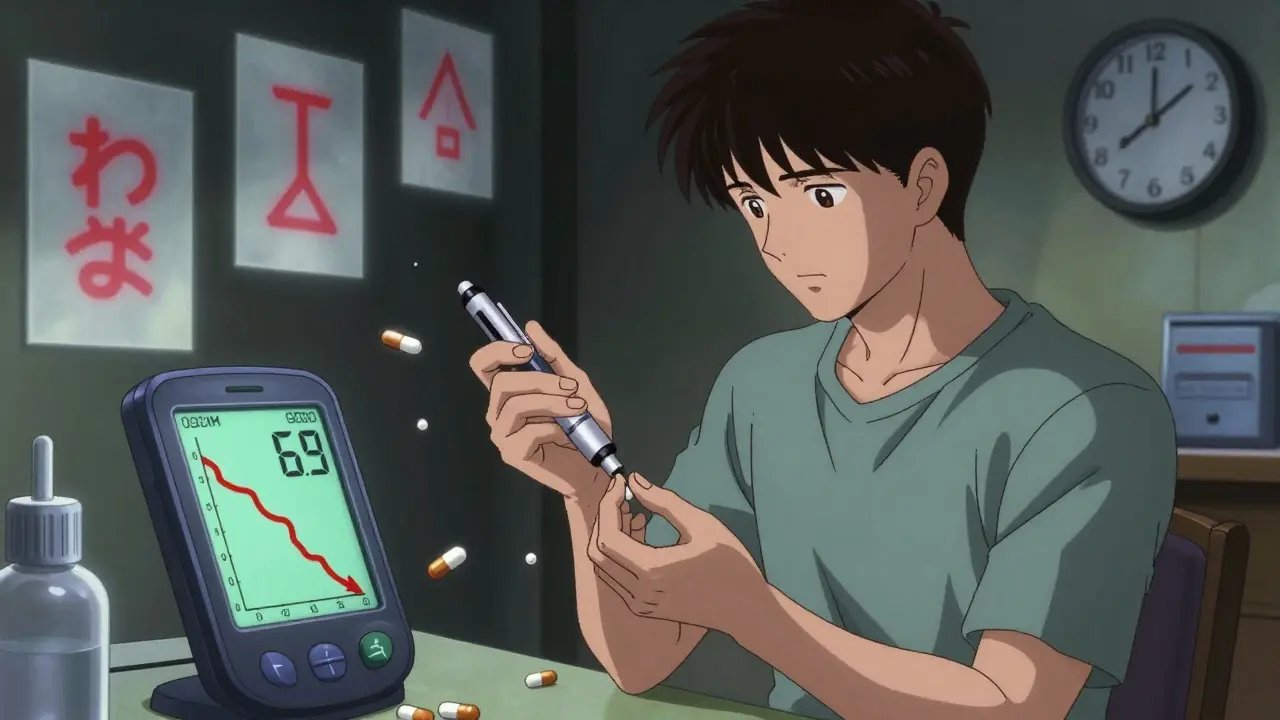
Start with at least four checks a day if you’re on 20 mg or more of prednisone. If your sugar goes above 180 mg/dL twice in a row, increase insulin. If it drops below 70 mg/dL, cut back.
Continuous glucose monitors (CGMs) cut guesswork. Studies show CGM users adjust insulin 37% more accurately than those using fingersticks. If you have one, use it. If you don’t, ask your doctor. It’s not a luxury-it’s a safety tool.
What Happens When Steroids Are Tapered?
This is where most people get hurt.
When steroids are lowered, your body starts making insulin again. But if your insulin dose hasn’t been reduced, you risk severe hypoglycemia. One study found 18% of hospital readmissions after steroid use were due to low blood sugar from unchanged insulin.
Here’s the rule: Reduce insulin as you reduce steroids.
For every 10 mg drop in prednisone equivalent, cut total daily insulin by 10-20%. Don’t wait until the steroid is gone. Start reducing when the dose drops below 20 mg. If you’re on 40 mg prednisone and drop to 30 mg, cut insulin by 10%. Go to 20 mg? Cut another 10%. Keep going.
And watch for symptoms: shaking, sweating, confusion, dizziness. These aren’t just signs of low sugar-they’re signs you didn’t adjust fast enough.
What About Oral Diabetes Medications?
Most oral meds don’t cut it with steroid hyperglycemia. Metformin? It helps a little with insulin resistance, but won’t handle the insulin shortage. SGLT2 inhibitors? Risk of dehydration and ketoacidosis goes up with steroids. DPP-4 inhibitors? Too weak.
Insulin is the gold standard. But if you’re on low-dose steroids (under 10 mg prednisone) and have mild type 2 diabetes, your doctor might try adding a GLP-1 agonist like semaglutide. It helps with insulin secretion and appetite-but it’s not first-line here.
For most, insulin is the only reliable tool. The rest are bandaids on a broken pipe.
Technology and Tools That Help
Some hospitals now use systems like EndoTool or Glytec’s eGlucose Management System. These tools link steroid doses to insulin recommendations in real time. In one trial, they cut hypoglycemia by 33% during steroid tapering.
Machine learning is stepping in too. A 2023 study showed an algorithm using steroid dose, BMI, and HbA1c could predict insulin needs with 85% accuracy. That’s not science fiction-it’s happening now in major medical centers.
Even if your hospital doesn’t use these tools, you can still use apps to log your glucose, steroid dose, and insulin. Look for patterns. Did your sugar spike every time you took your steroid at 8 a.m.? That’s your clue.
Common Mistakes to Avoid
- Only checking fasting glucose: You’ll miss 15-20% of hyperglycemia episodes.
- Not reducing insulin during taper: This is the #1 cause of dangerous low blood sugar after steroids.
- Using sliding scale alone: It’s reactive, not proactive. You’re always playing catch-up.
- Assuming steroids are temporary so you don’t need a plan: Even a 5-day course can cause dangerous spikes.
- Ignoring magnesium levels: Low magnesium makes everything worse. Ask for a blood test if you’re on long-term steroids.
What to Do If You’re Starting Steroids
If you’re about to start steroids and have diabetes:
- Call your endocrinologist or diabetes care team before your first dose.
- Get a CGM if you don’t have one.
- Know your steroid dose and schedule. Is it once daily? Twice? What time?
- Write down your current insulin doses and glucose targets.
- Plan your first 48 hours: check glucose 6-8 times a day.
- Have fast-acting carbs on hand in case your sugar drops too fast during taper.
Don’t wait for your sugar to hit 300 mg/dL. Get ahead of it. Steroid hyperglycemia is predictable. You don’t have to suffer through it.
Long-Term Outlook
For many, steroid hyperglycemia is temporary. Once the steroids stop, blood sugar often returns to normal. But for some-especially those with prediabetes or obesity-it can become permanent type 2 diabetes.
That’s why managing it right matters. Every episode of uncontrolled hyperglycemia stresses your pancreas, your blood vessels, your kidneys. You’re not just avoiding a bad day-you’re protecting your long-term health.
By 2027, nearly three-quarters of U.S. hospitals will have formal protocols for steroid hyperglycemia. But until then, you need to be your own advocate. Know the risks. Know the signs. Know how to adjust. Your body will thank you.

Ajay Brahmandam
December 21, 2025 AT 21:57Jeremy Hendriks
December 22, 2025 AT 11:24Jim Brown
December 23, 2025 AT 12:33Julie Chavassieux
December 25, 2025 AT 01:39Cara Hritz
December 26, 2025 AT 17:47jenny guachamboza
December 27, 2025 AT 21:23Gabriella da Silva Mendes
December 27, 2025 AT 21:24Tarun Sharma
December 29, 2025 AT 10:58Johnnie R. Bailey
December 29, 2025 AT 11:08Nader Bsyouni
December 30, 2025 AT 20:34Jamison Kissh
December 31, 2025 AT 23:50