When you start treatment for osteoporosis, you want to know if it’s working-fast. Waiting a year or two for a DXA scan to show if your bone density improved feels like guessing. That’s where bone turnover markers come in. They give you real-time feedback, often within weeks, not years. No radiation. No long waits. Just a simple blood test that tells you whether your meds are doing their job.
What Are Bone Turnover Markers?
Bone isn’t static. It’s constantly being broken down and rebuilt. That’s called remodeling. When bone breaks down, bits of collagen and other proteins spill into your blood and urine. When new bone forms, other proteins are released. These are bone turnover markers (BTMs). They’re like smoke signals from your skeleton-telling you how active your bone remodeling is.
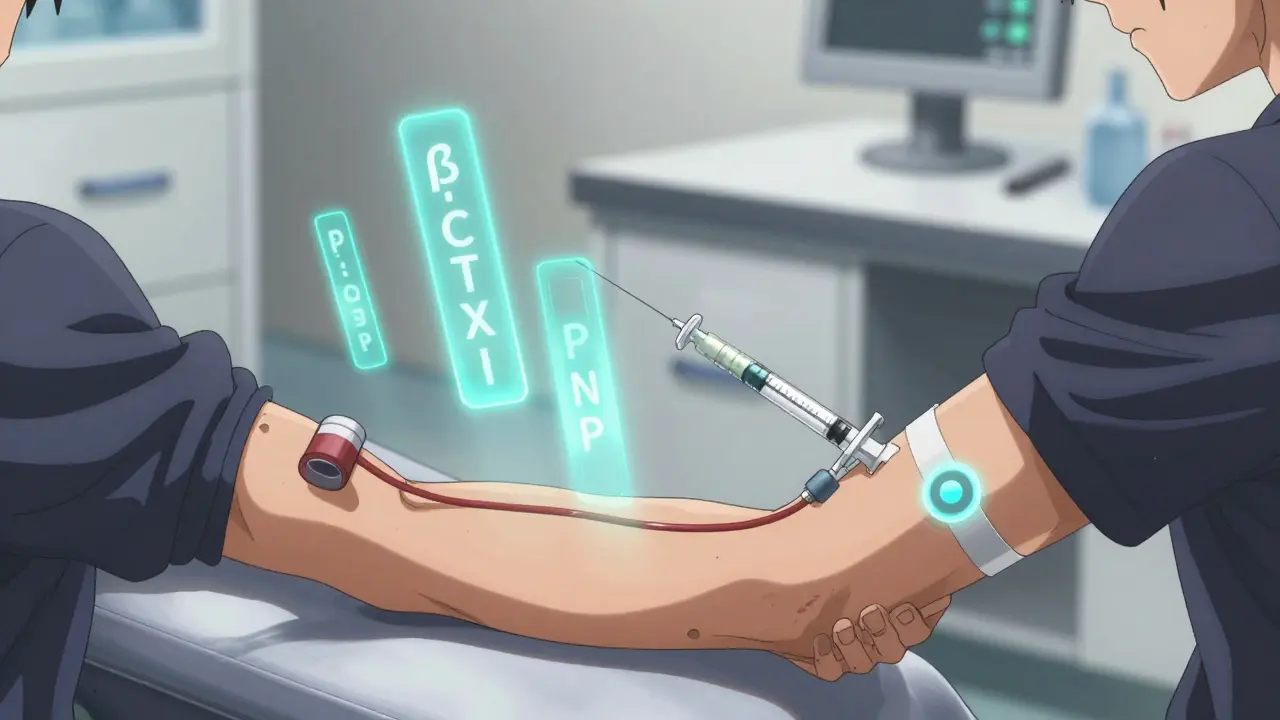
There are two main types:
- Resorption markers: Show how fast bone is being broken down. The best one is β-CTX-I (beta-C-terminal telopeptide of type I collagen). It’s measured in plasma and drops when you take drugs like bisphosphonates or denosumab.
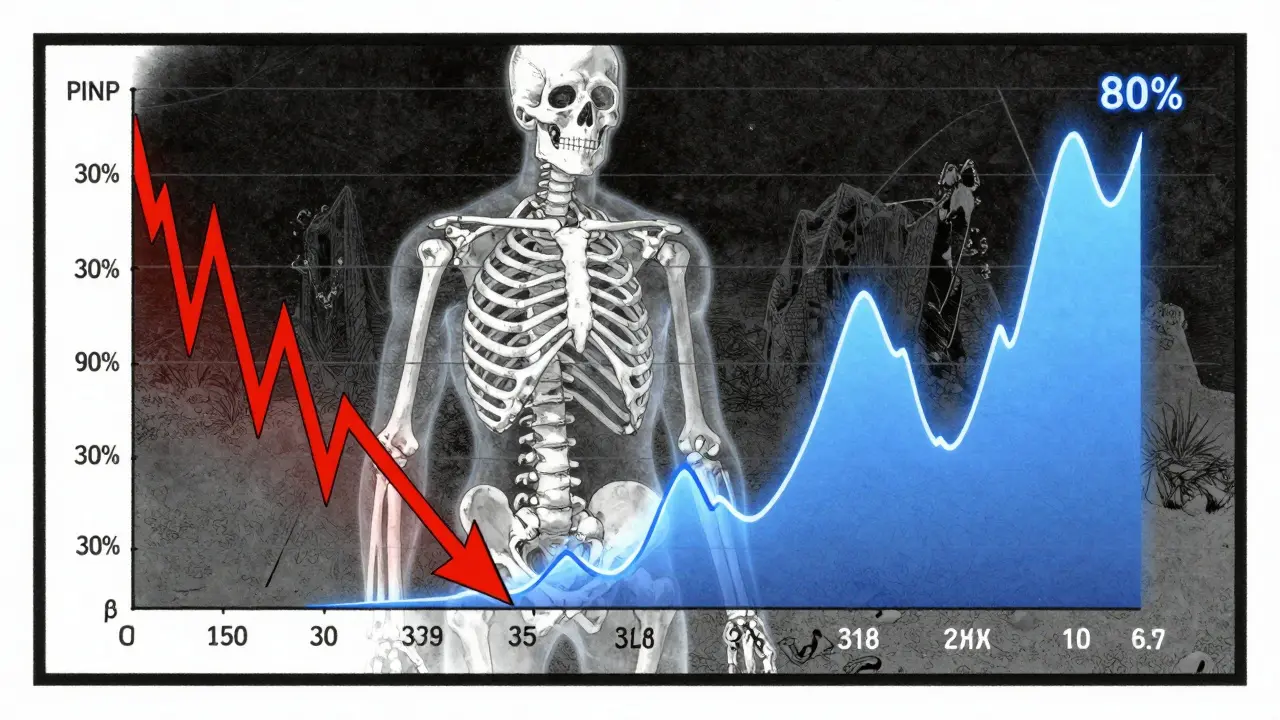
- Formation markers: Show how fast new bone is being made. The gold standard here is PINP (procollagen type I N-terminal propeptide). It rises when you use anabolic drugs like teriparatide.
These aren’t just lab curiosities. They’re validated by the International Osteoporosis Foundation and European Calcified Tissue Society as the most reliable markers for clinical use. Other markers like osteocalcin or urinary NTx exist, but they’re less consistent. PINP and β-CTX-I are the ones doctors trust.
Why Use Them Instead of Just Waiting for a DXA Scan?
DXA scans measure bone mineral density (BMD). They’re great for diagnosing osteoporosis and checking long-term progress. But they’re slow. It takes 12 to 24 months to see a meaningful change in BMD-even if the treatment is working perfectly.
Bone turnover markers change much faster. You can see a drop in β-CTX-I within 3 to 6 weeks of starting an anti-resorptive drug. PINP starts rising in just 1 to 3 months if you’re on teriparatide. That’s not a guess. That’s proof your body is responding.
Think of it this way: DXA tells you how strong your house is. BTMs tell you if the builders are showing up every day to fix the walls. If the builders aren’t there, you don’t wait two years to find out-you check the site after a week.
How Do You Know If the Treatment Is Working?
It’s not enough to just test. You need to know what the numbers mean.
For anti-resorptive drugs (like alendronate, risedronate, or denosumab):
- A 30% or greater drop in β-CTX-I within 3 to 6 months means you’re responding well.
- For PINP, a 35% or greater drop is the target.
For anabolic drugs (like teriparatide or romosozumab):
- PINP should rise by 70% to 100% within 3 months.
- β-CTX-I may rise slightly too, but PINP is the key signal.
There’s a catch: not every change means something. Biological noise and lab variation can cause small fluctuations. That’s why labs use the least significant change (LSC). For PINP, it’s 20%. For β-CTX-I, it’s 25%. If your result changes less than that, it’s probably just random variation-not a real response.
And here’s the kicker: patients who hit these targets in the first 3 months have a 1.6% lower fracture risk after 22 weeks, according to the TRIO study. That’s not a small win. That’s life-changing.
When and How Should You Test?
Testing isn’t random. It’s timed. Mess up the timing, and your results are useless.
For β-CTX-I (the resorption marker):
- Must be done in the morning, between 8 and 10 AM.
- You need to be fasting-no food or drink (except water) for at least 8 hours.
- Even a light breakfast can raise β-CTX-I by 20-30%.
- Diurnal variation (natural daily swings) can be as high as 40% if you test at the wrong time.
For PINP:
- Less affected by meals or time of day.
- Still best to test in the morning for consistency.
- Diurnal variation is only 10-15%.
Here’s the standard protocol:
- Test both PINP and β-CTX-I before starting treatment to get your baseline.
- Repeat the test 3 months after starting therapy.
- Compare the new numbers to your baseline using the LSC and response thresholds.
- Don’t test again until 6-12 months unless there’s a reason to suspect non-adherence or poor response.
Skipping the baseline? That’s like measuring your weight after starting a diet but never knowing your starting point. You can’t tell if you lost anything.
Who Should Get Tested?
Not everyone needs BTMs. But they’re most useful in these cases:
- Patients starting new osteoporosis therapy-especially if they’re on anabolic drugs.
- People with poor adherence-if you’re not taking your pills, BTMs will show it.
- Those with high fracture risk and need quick feedback to adjust treatment.
- Patients with chronic kidney disease-standard markers like PINP and β-CTX-I can be skewed by poor kidney function. In these cases, bone alkaline phosphatase (BALP) or TRACP5b may be better.
- Anyone who’s not responding to treatment after 6 months and you need to know why.
For someone just diagnosed and starting on a bisphosphonate, BTMs can be a game-changer. If their β-CTX-I doesn’t drop by 30% at 3 months, they’re likely not taking the pill. Or maybe they’re taking it wrong-like with coffee or calcium supplements. That’s something you can fix. No need to wait 2 years to find out.
Limitations and Pitfalls
Bone turnover markers aren’t perfect. They’re tools, not crystal balls.
First, they measure systemic bone turnover. They don’t tell you what’s happening in your spine or hip specifically. That’s why DXA still rules for diagnosis and long-term tracking.
Second, biological variability is high. Your levels can jump up or down due to stress, illness, menstrual cycle, or even recent exercise. That’s why you need baseline and repeat testing under the same conditions.
Third, lab methods matter. Not every lab uses the same test. The IFCC and IOF recommend specific assays from Roche or Siemens. If your lab uses an older ELISA method, results might not line up with published guidelines. Ask your doctor: “Which assay are you using?”
Fourth, reference ranges vary by population. Most data comes from Caucasian women. Asian populations tend to have 15-20% lower baseline β-CTX-I. African populations have higher PINP. If you’re not Caucasian, your “normal” might be different. Labs need to adjust for that.
And finally, BTMs are useless if the sample is mishandled. A blood tube left in the sun or shaken too hard can destroy the markers. That’s why labs need trained staff. And why your doctor should know the protocol.
What’s Next for Bone Turnover Markers?
The science is evolving. In 2023, the IOF, ESCEO, and IFCC all agreed: PINP and β-CTX-I are the reference markers. But they’re pushing for more research.
Trials are underway to see if using BTMs to guide treatment-like switching drugs early if there’s no response-can reduce fractures even more. One trial (NCT04567821) is testing whether patients who hit their BTM targets have fewer fractures over 5 years.
Point-of-care tests are coming. Imagine getting your BTM result in your doctor’s office in 20 minutes, not 5 days. The FDA hasn’t approved them yet, but companies are close.
Insurance coverage is improving. Medicare in the U.S. pays for PINP and β-CTX-I tests. In Europe, up to 60% of clinics use them routinely. In the U.S., adoption is still around 30%, but it’s rising.
And the cost? It’s low. Around $30 per test. Compare that to a hip fracture-$50,000 in hospital bills, plus rehab, lost independence, and risk of death. One test, $30. A fracture, $50,000. The math is clear.
Bottom Line
Bone turnover markers aren’t magic. But they’re the fastest, most direct way to know if your osteoporosis treatment is working. They turn guesswork into data. They help catch non-adherence before it leads to fractures. They give you and your doctor confidence-early.
If you’re on osteoporosis meds, ask your doctor: “Can we check my PINP and β-CTX-I before I start, and again in 3 months?” If they say no, ask why. The evidence is solid. The guidelines are clear. The tools are available. You deserve to know if your treatment is working-not wait two years to find out.
Blow Job
December 25, 2025 AT 03:01Finally, someone explains this without jargon overload. I’ve been on denosumab for 8 months and my doc never mentioned BTMs-until now. I’m scheduling my PINP and β-CTX-I test next week. If it shows I’m not responding, I’m switching meds. No more guessing.
Christine Détraz
December 26, 2025 AT 09:32This is the kind of post that makes me feel less alone in this. My mom had a vertebral fracture last year, and the whole process felt like flying blind. I printed this out and gave it to her rheumatologist. She actually listened. Small wins, right?
Ajay Sangani
December 27, 2025 AT 05:48bone is alive… i never thought of it that way. like a forest that’s always growing and falling down. we think of bones as static, like stone. but they’re not. they’re breathing. maybe that’s why we feel so broken when we fracture. we’re not just losing structure-we’re losing rhythm.
Pankaj Chaudhary IPS
December 28, 2025 AT 15:28In India, access to these tests remains a luxury. Most clinics still rely on DXA alone. But this is the future. We need policy makers to recognize that spending $30 now prevents $50,000 later. Osteoporosis isn’t just a women’s issue-it’s a public health crisis waiting to explode as our population ages.
Aurora Daisy
December 29, 2025 AT 13:28Oh wow. So the American medical system finally caught up to the fact that people don’t want to wait two years to know if their pills are working? Took long enough. Meanwhile, in the UK, we’ve been doing this since 2017. Guess we’re just ahead of the curve.
Paula Villete
December 30, 2025 AT 09:01soooo… if i take my bisphosphonate with coffee and then get my β-CTX-I tested at noon after eating a bagel… am i just wasting my money? because i might be. oops. my doc never told me. thanks internet stranger.
Georgia Brach
December 30, 2025 AT 17:54Let’s be real. These markers are useful, but they’re not a magic bullet. Labs are inconsistent. Doctors misinterpret them. Patients don’t follow protocols. And now we’re supposed to trust a number that can swing 25% due to stress or sleep? This feels like medical theater dressed up as science.
Katie Taylor
December 31, 2025 AT 05:48MY DOCTOR DIDN’T EVEN KNOW ABOUT PINP. I HAD TO GOOGLE IT. THEN I PRINTED THIS POST AND TAPED IT TO HIS DESK. HE’S SCHEDULING MY TESTS TOMORROW. IF YOU’RE ON OSTEOPOROSIS MEDS AND YOUR DOCTOR HASN’T MENTIONED BTMS-FIGHT FOR IT.
Isaac Bonillo Alcaina
January 1, 2026 AT 16:19You people are acting like this is revolutionary. It’s not. It’s just another way for pharma to sell more tests. The real solution is vitamin D, weight-bearing exercise, and stopping smoking. This is just expensive noise.
suhani mathur
January 2, 2026 AT 11:11And yet, 90% of patients don’t get tested because their docs don’t order it. Why? Because insurance won’t cover it unless you’re in a trial. Or because they’re too busy to explain it. So we’re left with the lucky few who know to ask. That’s not healthcare. That’s a lottery.
Diana Alime
January 3, 2026 AT 21:13i just found out i have osteoporosis. i’m 42. i’m not old. i’ve been lifting weights since college. i don’t smoke. i drink milk. so why? and now i’m supposed to get a blood test that i don’t even understand? this feels like a trap. why does my body hate me??
Usha Sundar
January 4, 2026 AT 04:24Test at 8 AM. Fast. No coffee. PINP and β-CTX-I. Repeat in 3 months. If it doesn’t move, change meds. That’s it. No fluff. Just do it.