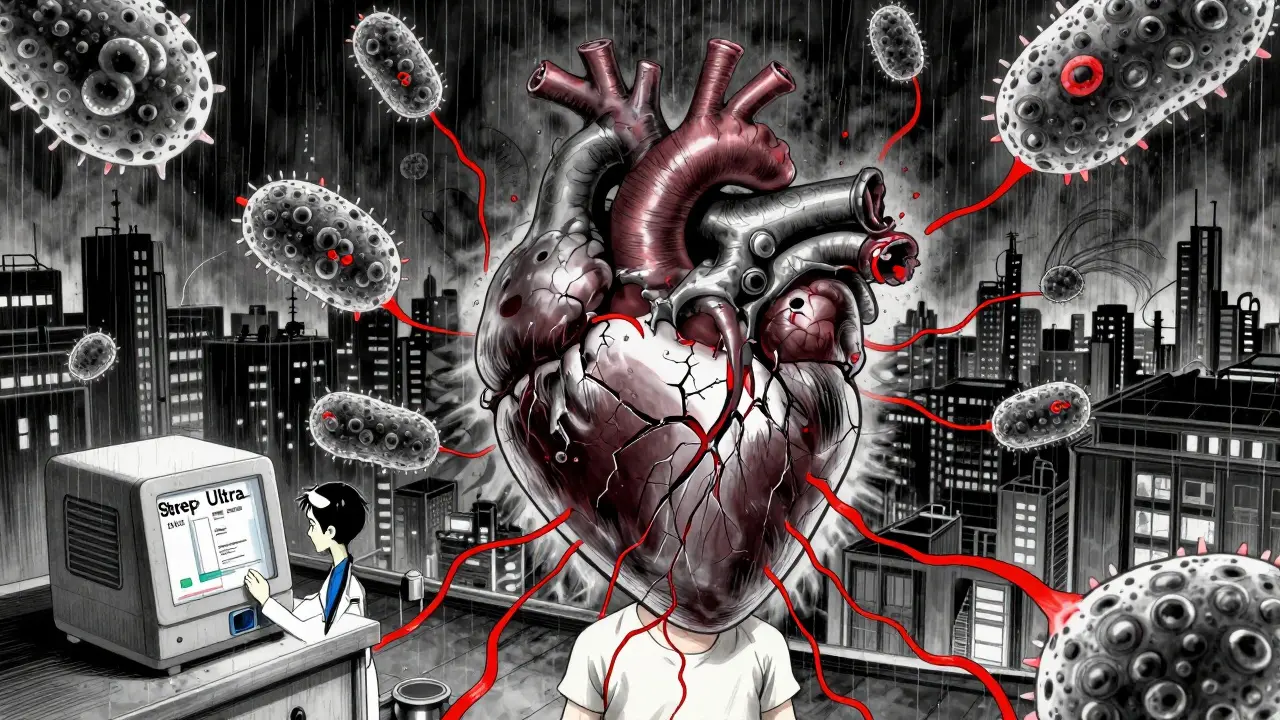
Strep throat isn’t just a sore throat. It’s a bacterial infection caused by Group A Streptococcus (Streptococcus pyogenes) - and if left untreated, it can lead to serious complications like rheumatic fever, which damages the heart valves. Unlike viral sore throats that come with coughing and runny noses, strep throat hits hard and fast, often without warning. It’s most common in kids between 3 and 9 years old, but teens and adults can get it too. The key is knowing when it’s strep - and what to do next.
How to Tell If It’s Strep Throat - Not a Cold
Not every sore throat is strep. In fact, most are viral. But there are clear signs that point to bacterial infection. The biggest clue? Absence of cough. If you or your child has a sore throat but no cough, no runny nose, and no sneezing, that’s a red flag for strep. According to UC Davis Health, this combination has over 90% specificity for strep throat.
Other classic symptoms include:
- Sudden, severe throat pain
- Fever above 100.4°F (38°C)
- White patches or pus on the tonsils
- Tender, swollen lymph nodes in the neck
- Small red spots on the roof of the mouth (palatal petechiae)
- Headache or stomach pain (especially in kids)
Doctors use something called the Centor criteria a scoring system that assigns points for fever, absence of cough, swollen lymph nodes, and tonsil exudate. If you score 3 or more points, there’s a 40-60% chance you have strep. That’s when testing becomes necessary.
Testing for Strep Throat: Rapid Test, Culture, or PCR?
There’s no way to diagnose strep just by looking. You need a test. Three main options exist:
- Rapid Antigen Detection Test (RADT): This gives results in 10-30 minutes. It’s accurate - over 95% specific - but misses about 5-15% of cases, especially in young kids. It’s the go-to first step in most clinics.
- Throat Culture: The gold standard. Swabs are sent to a lab and grown for 18-48 hours. It catches nearly all cases (90-95% sensitivity) and is required if the rapid test is negative in children or teens.
- Molecular (PCR) Test: Newer, faster, and more sensitive. Detects bacterial DNA with 95-98% accuracy. Turnaround is 24-48 hours. Some urgent care centers now use this as their primary test, especially since the FDA approved a new 15-minute version called Strep Ultra in March 2024.
Guidelines differ slightly. The CDC says: if a child or teen tests negative on a rapid test, follow up with a culture. For adults with low symptoms, no further testing is needed. But in practice, many doctors test everyone with classic symptoms - better safe than sorry.
Antibiotics: What Works, What Doesn’t
Strep throat responds well to antibiotics - but only if you pick the right one and take it fully. The Infectious Diseases Society of America (IDSA) updated its guidelines in 2022 to reflect rising resistance and now recommends:
- First-line: Penicillin V - 500 mg twice daily for adults, 250 mg twice daily for kids. Or amoxicillin - 50 mg/kg once daily (max 1000 mg), or 25 mg/kg twice daily (max 500 mg per dose). Both are 95% effective at clearing the bacteria.
- For penicillin allergies: Cephalexin, clindamycin, or azithromycin. These are slightly less effective (85-90%) and carry higher risk of side effects or resistance.
Why 10 days? Because shorter courses - even 5-day regimens - have higher relapse rates. The CDC reports 5-15% of untreated cases lead to relapse. And relapse isn’t just uncomfortable - it increases the chance of rheumatic fever.
Cost matters too. Generic penicillin V costs as little as $4. Azithromycin (brand-name Zithromax) can hit $250. Most insurance covers the cheap options. Never use leftover antibiotics from past illnesses - it fuels resistance.
Recovery Timeline: What to Expect
With antibiotics, you’ll feel better fast - but not overnight.
- 24-48 hours: Fever drops, throat pain eases. You’re no longer contagious. Kids can return to school. Adults can go back to work.
- 3-5 days: Most symptoms vanish. Swallowing becomes easy again.
- 7-10 days: Full recovery. Even if you feel fine, finish the full course. Stopping early is the #1 reason strep comes back.
Without antibiotics, symptoms last 7-10 days - but you stay contagious the whole time. And you risk complications like peritonsillar abscess (a pus-filled pocket near the tonsil) or rheumatic fever. The CDC says untreated strep leads to rheumatic fever in about 3% of cases - a disease that can permanently damage the heart.
Why Compliance Matters More Than You Think
Here’s the ugly truth: nearly 40% of parents stop antibiotics as soon as the fever breaks. That’s a mistake. A 2023 study in JAMA Pediatrics showed kids who stopped early had a 3x higher chance of relapse.
Other risky behaviors:
- Sharing antibiotics (8% of adults on Reddit admitted to it in January 2024)
- Using old prescriptions (12% of CDC survey respondents)
- Not replacing toothbrushes after treatment (bacteria can linger)
Compliance is everything. Studies show 95% of people who finish their full course clear the infection. Only 85% do if they quit early. That 10% gap is why we still see rheumatic fever cases - mostly in communities where treatment adherence is low.
When to Worry: Red Flags After Starting Antibiotics
Most people improve quickly. But if you or your child still has:
- Fever after 48 hours of antibiotics
- Difficulty swallowing or breathing
- Swelling in the neck or jaw
- Severe headache, rash, or joint pain
Call your doctor. You might have a complication like a peritonsillar abscess (1-2% of cases) or a secondary infection. Rarely, strep can trigger scarlet fever or post-streptococcal glomerulonephritis (kidney inflammation). Early detection saves lives.
Prevention and Future Outlook
Strep spreads through droplets - coughs, sneezes, shared cups. Wash hands. Don’t share utensils. Replace toothbrushes after 24 hours of antibiotics.
There’s no vaccine yet. The M-protein vaccine a candidate for Group A strep is in Phase II trials, but with over 200 strains circulating, it’s a tough target. For now, prevention comes down to smart diagnosis and full antibiotic courses.
Looking ahead, point-of-care PCR tests will likely become standard in urgent care centers by 2026. The CDC has allocated $15 million to track resistance patterns. But the biggest challenge remains: getting people to finish their pills.
Can you get strep throat without a fever?
Yes, though it’s rare. Fever is present in about 85% of confirmed cases. Some adults, especially those with weaker immune systems, may have sore throat and swollen glands without a high fever. But if you have no fever, no pus, and no swollen lymph nodes, it’s more likely viral.
Is strep throat contagious after 24 hours of antibiotics?
No. Once you’ve taken antibiotics for at least 24 hours and your fever is gone, you’re no longer contagious. That’s why kids can return to school after one full day of treatment - as long as they’re feeling better.
Can adults get strep throat more than once?
Yes. Unlike chickenpox, getting strep once doesn’t give lifelong immunity. You can get it again - even within the same season. That’s why it’s critical to complete your full antibiotic course and avoid exposure during outbreaks.
Why not just treat all sore throats with antibiotics?
Because most sore throats are viral. Antibiotics don’t work on viruses. Using them unnecessarily drives antibiotic resistance - which is why the CDC says 30% of outpatient antibiotic prescriptions are unnecessary. Testing ensures we only treat what needs treatment.
What if I’m allergic to penicillin? Are there safe alternatives?
Yes. For mild penicillin allergies, cephalexin is often safe. For true allergies, clindamycin or azithromycin are options. But azithromycin has higher resistance rates in some areas (up to 15%), so it’s not always reliable. Always tell your doctor your allergy history - never guess.
Do rapid strep tests work for toddlers?
They can, but they’re less reliable in kids under 5. Bacterial load is lower in younger children, leading to more false negatives. If symptoms are classic and the rapid test is negative, most pediatricians still order a throat culture to be sure.

Michaela Jorstad
February 19, 2026 AT 19:10As someone who’s been through this twice with my daughter, I can’t stress enough: finish the whole damn course. Even when she seemed fine at day three, I made her keep going. No compromises. I’ve seen too many parents stop early because ‘they’re better’-and then it comes back worse. Seriously, don’t gamble with rheumatic fever. Penicillin’s $4. Your kid’s heart? Priceless.