When you’re living with Crohn’s disease or ulcerative colitis, everyday life can feel like a constant battle. Fatigue, pain, frequent bathroom trips - these aren’t just inconveniences. They’re symptoms of your immune system attacking your own gut. For many, standard treatments like steroids or immunomodulators don’t cut it anymore. That’s where IBD biologics come in. These aren’t your average pills. They’re precision-targeted drugs designed to silence specific parts of your immune system that are causing the damage.
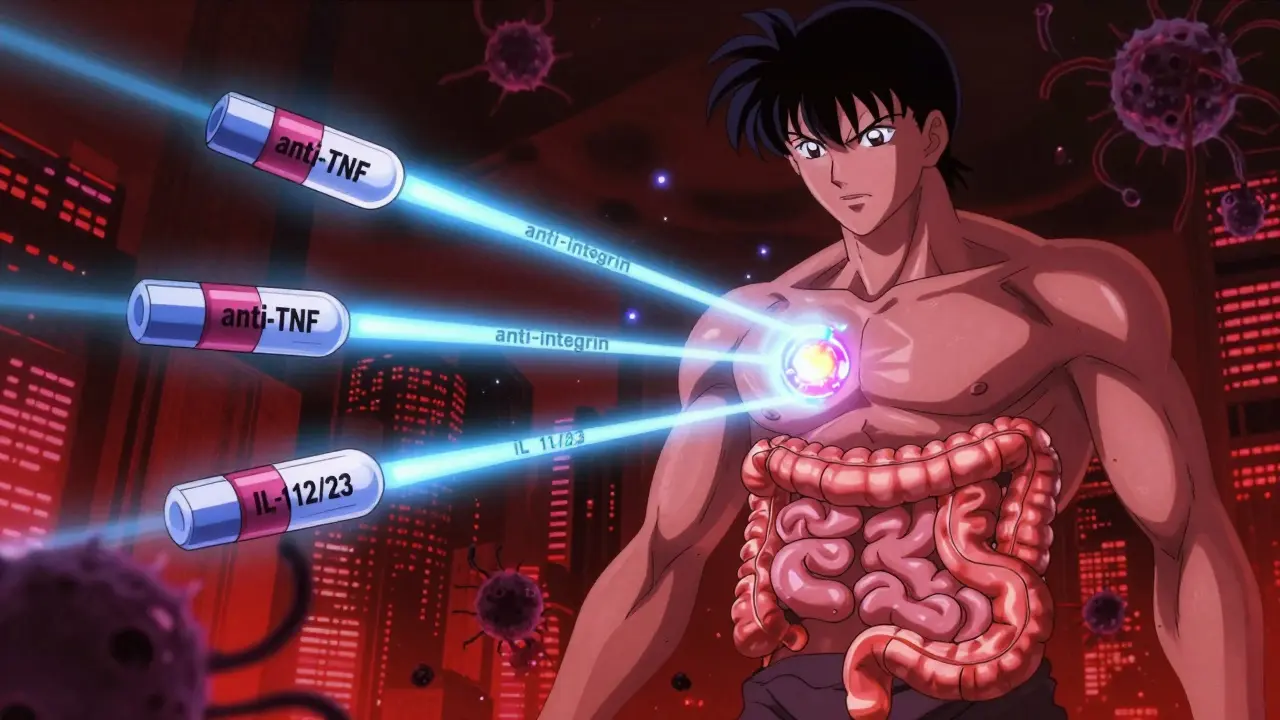
What Are IBD Biologics and How Do They Work?
IBD biologics are made from living cells, not chemicals. They mimic proteins your body naturally produces to calm down overactive immune responses. Instead of broadly suppressing your entire immune system - which leaves you vulnerable to infections - these drugs pick out one specific target. Think of them like sniper rifles instead of shotguns.
There are three main types in use today: anti-TNF agents, anti-integrin therapies, and IL-12/23 inhibitors. Each one blocks a different signal that tells your immune system to attack your intestines. They’re not cures, but for many people, they’re life-changing. Studies show they can reduce flare-ups, heal gut lining, and cut hospital visits by more than half.
Anti-TNF Inhibitors: The First Line of Defense
Anti-TNF drugs were the first biologics approved for IBD, starting with infliximab (Remicade) in 1998. They block tumor necrosis factor-alpha, a key inflammatory messenger. Today, four are available: infliximab, adalimumab (Humira), golimumab (Simponi), and certolizumab pegol (Cimzia).
Infliximab is given as an IV infusion - usually at a clinic - at weeks 0, 2, and 6, then every 8 weeks after that. Each session takes 2 to 4 hours. Adalimumab is a self-injection you give under your skin every other week. Many patients prefer the convenience of injections, but infliximab has stronger evidence for deep healing.
According to a 2022 meta-analysis, infliximab leads in clinical remission and mucosal healing for patients who’ve never used a biologic before. It outperforms adalimumab in both areas. But here’s the catch: adalimumab’s real advantage is accessibility. You can do it at home. No clinic trips. No IV lines. For someone with a busy job or long commute, that matters.
Side effects? Common ones include injection site reactions for adalimumab and infusion reactions for infliximab. More serious risks include tuberculosis reactivation and increased risk of lymphoma. That’s why everyone gets a TB test before starting. Biosimilars like Inflectra and Cyltezo now make these drugs more affordable, cutting costs by 15-30%.
Anti-Integrin Therapies: Gut-Selective and Safer
Vedolizumab (Entyvio) is the only anti-integrin drug currently approved for IBD. It works differently. Instead of shutting down inflammation system-wide, it blocks white blood cells from entering the gut. That’s why it’s called “gut-selective.”
It’s given as an IV infusion, same schedule as infliximab. But here’s the big win: fewer systemic side effects. Unlike anti-TNFs, vedolizumab doesn’t increase your risk of serious infections or neurological issues like PML (a rare brain infection linked to another drug, natalizumab). That makes it ideal for patients with a history of MS, latent TB, or those who’ve had bad reactions to TNF blockers.
On MyIBDTeam, 72% of users report vedolizumab is effective. But 44% say it takes too long to work - 6 to 10 weeks before they feel better. That’s slower than anti-TNFs, which often kick in within 2 to 4 weeks. Still, patients who’ve tried both often switch to vedolizumab after losing response to TNF inhibitors. One Reddit user wrote: “Switched from Humira to Entyvio after five years. No more weekly injections. But I waited 10 weeks to feel relief. Brutal.”
Cost-wise, a single 300mg dose runs around $5,500. But manufacturer assistance programs often bring out-of-pocket costs to $0 for insured patients.
IL-12/23 and IL-23 Inhibitors: The New Generation
Ustekinumab (Stelara) was the first IL-12/23 inhibitor approved for IBD, hitting the market in 2016 for Crohn’s and 2019 for ulcerative colitis. It blocks two inflammatory proteins - IL-12 and IL-23 - that drive chronic gut inflammation.
It’s a subcutaneous injection, given every 8 or 12 weeks depending on your weight. Patients like it because it’s less frequent than adalimumab and doesn’t require clinic visits. Studies show it works well for those who didn’t respond to TNF inhibitors. About 60% of patients achieve clinical remission after a year.
Then came the IL-23-only inhibitors: risankizumab (Skyrizi) and mirikizumab (Omvoh). Risankizumab got FDA approval for ulcerative colitis in June 2024 - a big deal. It’s now approved for both Crohn’s and UC. In trials, 29% of UC patients were in remission at 52 weeks, compared to just 10% on placebo.
These drugs are fast-acting, safe, and have minimal infection risk. They’re becoming the go-to for patients who want strong results without the long-term dangers of TNF blockers. Experts predict IL-23 inhibitors will make up 30% of the IBD biologic market by 2028.
Which One Is Right for You?
There’s no one-size-fits-all answer. Your choice depends on your disease severity, lifestyle, risk factors, and past treatment history.
- If you need quick results and have moderate to severe disease, infliximab still has the strongest evidence.
- If you hate clinics and can handle weekly injections, adalimumab is convenient - even if it’s slightly less effective.
- If you’ve had infections, TB, or neurological issues, vedolizumab is the safest bet.
- If you failed TNF inhibitors or want fewer side effects long-term, ustekinumab or risankizumab are top choices.
Doctors often start with anti-TNFs because they’ve been around the longest and have the most data. But that’s changing. Many now consider vedolizumab or ustekinumab as first-line for patients with psoriasis (TNF blockers can make it worse) or those who travel often.
Real-Life Challenges: Cost, Convenience, and Compliance
Even the best drug won’t help if you can’t take it.
Costs are steep. A single dose of ustekinumab can hit $7,200. But most patients pay little or nothing thanks to manufacturer assistance programs. Janssen CarePath and AbbVie’s programs help 95% of eligible patients get their meds for $0-$5 per dose.
Time is another hurdle. Infusion therapies mean 3-5 hours every 8 weeks. That’s a full day gone - driving, waiting, recovering. One patient told a survey: “The 8-hour round trip to the infusion center every 8 weeks is unsustainable.”
Injection anxiety is real. About 22% of patients on adalimumab need counseling to get past fear of needles. Apps like MyTherapy help track doses and send reminders. Sixty-eight percent of users say it improves adherence.
And then there’s the fear of long-term side effects. Many patients worry about cancer or infections. The truth? The risks are real but low. For most, the benefits outweigh the dangers - especially when you’re avoiding hospitalizations and steroid dependence.
What’s Next? The Future of IBD Treatment
The pipeline is full. Etrolizumab, another anti-integrin drug, is in phase 3 trials. Mirikizumab is being tested for Crohn’s. Researchers are also looking at biomarkers - blood tests or stool markers - to predict which drug will work best for you before you even start.
Trials like RHEA and VEGA are comparing biologics head-to-head. Right now, most data comes from indirect comparisons - which can be misleading. By 2026, we’ll have clearer answers.
One thing’s certain: IBD treatment is becoming more personalized. No longer are we guessing. We’re matching the right drug to the right patient based on their biology, lifestyle, and goals.
By 2030, experts predict 60% of moderate-to-severe IBD patients will be on biologics. But access remains a problem. One in four patients still struggle to get insurance approval. That’s why patient advocacy groups like the Crohn’s & Colitis Foundation are pushing harder than ever for affordability and equity.
Brooks Beveridge
December 17, 2025 AT 04:38Man, I remember when I first started on Humira. Felt like I was fighting a war inside my gut every day. Then I switched to Entyvio after two years of constant flares. Took forever to kick in - like 10 weeks - but once it did? I could sleep through the night for the first time in years. No more panic attacks before leaving the house. This stuff isn’t magic, but it’s the closest thing we got.
Keep going, folks. It’s a grind, but you’re not alone.
Naomi Lopez
December 18, 2025 AT 19:09Let’s be real - anti-TNFs are the OGs, but they’re also the most overprescribed. I’ve seen patients on adalimumab for five years, losing response, then getting stuck in a loop of dose escalation while their liver enzymes climb. Meanwhile, IL-23 inhibitors like Skyrizi are showing 3x better mucosal healing in head-to-head trials. Why are we still treating this like it’s 2010?
Josh Potter
December 18, 2025 AT 22:06Bro I just got my first Stelara shot last week and I’m already feeling like a new person. No more 3 a.m. bathroom runs. No more ‘can I make it to the airport?’ anxiety. And the injection? Barely a pinch. I used to hate needles, now I’m like ‘yo, when’s my next one?’
PS: Janssen CarePath got me the whole thing for $0. If you’re struggling with cost, DM me. I’ll send you the link.
Marie Mee
December 20, 2025 AT 06:47They’re lying about the safety. I know a guy who got lymphoma after Humira. They say it’s rare but what if it’s you? And why do they always skip the part where the drug makes you sick for weeks before it works? They just want you to keep paying.
They’re not curing you. They’re keeping you hooked.
Sachin Bhorde
December 21, 2025 AT 16:16Guys, if u r on vedolizumab and it’s taking too long - don’t give up. It’s like planting a seed. You don’t see roots for weeks, but underground? It’s working. I was skeptical too. Took 8 weeks, but now I’m in remission for 14 months. No steroids, no ER visits. Just… life.
Also, biosimilars are legit. Inflectra saved me $4k/month. Pharma companies aren’t saints, but the system ain’t all evil. Fight for access, not against hope.
Evelyn Vélez Mejía
December 23, 2025 AT 07:10The paradigm shift here isn’t technological - it’s philosophical. We’ve moved from suppressing the immune system to silencing its specific screams. Anti-TNFs were a sledgehammer. IL-23 inhibitors are a tuning fork. We’re no longer treating inflammation; we’re listening to the gut’s dialect and responding in its own language.
What’s astonishing isn’t the efficacy - it’s that we finally stopped treating Crohn’s as a defect to be eradicated, and began honoring it as a signal to be understood. This is medicine becoming poetry.
Nishant Desae
December 23, 2025 AT 19:40I’ve been living with UC for 18 years and I’ve tried almost everything - steroids, azathioprine, even that weird trial drug that made me hallucinate. But ustekinumab? It’s the first thing that didn’t feel like a trade-off. I don’t feel like I’m being poisoned to feel better. I can travel now. I can eat pizza without planning my route to the nearest bathroom. I don’t cry every time I see my kid’s school photo because I missed their recital.
And yeah, it’s expensive - but if your insurance says no, call the foundation. They’ll help. I did. And I’m still here. You can be too. Don’t give up. The science is on your side.
Michael Whitaker
December 25, 2025 AT 17:31It’s amusing how the medical establishment still clings to anti-TNFs as first-line therapy when the data clearly favors gut-selective agents for long-term outcomes. The inertia is less about clinical efficacy and more about entrenched reimbursement structures and physician habituation. One must question whether we’re treating patients - or optimizing for billing codes and formulary compliance.
Furthermore, the absence of direct comparative trials before 2026 is a glaring methodological gap. We are prescribing based on indirect comparisons, which, statistically speaking, is akin to comparing apples to oranges while blindfolded.
Victoria Rogers
December 27, 2025 AT 01:08Why do we trust Big Pharma’s ‘safe’ labels when they hid the truth about opioids? Same playbook. They hype the ‘miracle drug’ then bury the long-term risks. IL-23 inhibitors? They’ve only been out 2 years. Who’s to say they won’t cause autoimmune liver damage in 10 years? They’re testing on us like lab rats.
And don’t get me started on ‘biosimilars’ - just knockoffs with the same side effects and a cheaper price tag. They’re not cheaper because they’re better. They’re cheaper because they’re copying.