When you hear the word biosimilar, you might think it’s just another generic drug. But that’s not true. Monoclonal antibody biosimilars aren’t copies like the pills you take for high blood pressure. They’re complex biological medicines made from living cells - and getting them right is one of the hardest tasks in modern medicine.
What Makes Monoclonal Antibody Biosimilars Different
Unlike small-molecule generics, which are chemically identical to their brand-name versions, biosimilars are highly similar but not exact copies. Why? Because monoclonal antibodies are huge proteins - about 150,000 daltons in size - made by living cells in bioreactors. Even tiny changes in temperature, pH, or nutrient mix during production can alter their structure slightly. These aren’t mistakes; they’re natural variations, like fingerprints on a snowflake. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) both require proof that these differences don’t affect safety, purity, or how well the drug works. That means biosimilar makers must run hundreds of lab tests, animal studies, and clinical trials to show their product matches the original - the reference product - in every meaningful way. One key area they watch closely is glycosylation. That’s the process where sugar molecules attach to the antibody. Change the sugar pattern, and you might trigger an immune reaction. In rare cases, patients given cetuximab (a cancer drug) had severe allergic reactions because their bodies recognized a specific sugar structure - alpha-1,3-galactose - as foreign. This isn’t common, but it shows why biosimilars can’t be treated like simple generics.Approved Monoclonal Antibody Biosimilars and Their Uses
Since 2013, dozens of monoclonal antibody biosimilars have been approved worldwide. Here are the most common ones and what they treat:- Bevacizumab biosimilars (Avastin): Used for colorectal, lung, ovarian, and brain cancers. Six versions are approved in the U.S., including Mvasi, Zirabev, and Vegzelma.
- Rituximab biosimilars (Rituxan): Treats non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and rheumatoid arthritis. Truxima, Ruxience, and Riabni are the three approved in the U.S.
- Trastuzumab biosimilars (Herceptin): Targets HER2-positive breast and stomach cancers. Six biosimilars are available, including Ogivri, Herzuma, and Kanjinti.
- Infliximab biosimilars (Remicade): Used for Crohn’s disease, ulcerative colitis, and rheumatoid arthritis. Remsima became the first monoclonal antibody biosimilar to get FDA interchangeability status in July 2023.
- Adalimumab biosimilars (Humira): The most prescribed biologic in the world. Fourteen biosimilars are in development or approved, including Hyrimoz, approved in September 2023.
Real-World Impact: Cost Savings and Patient Outcomes
A 2022 study in JAMA Oncology tracked 1,247 patients with lymphoma who switched from reference rituximab to Truxima. The results? No drop in effectiveness. No increase in side effects. And a 28% drop in cost per treatment cycle. That’s not just a number - it’s a patient who can afford more cycles, or one less financial burden on their family. The numbers add up fast. Evaluate Pharma predicts biosimilar monoclonal antibodies will save the U.S. healthcare system $250 billion between 2023 and 2028. Bevacizumab, trastuzumab, and rituximab biosimilars will make up 78% of those savings. Even more impressive? The FDA has approved six biosimilars for filgrastim (used to boost white blood cells after chemo) and one for epoetin alfa (used to treat anemia). These aren’t flashy cancer drugs - they’re supportive care. But they’re just as vital. Without them, many patients couldn’t complete their treatment.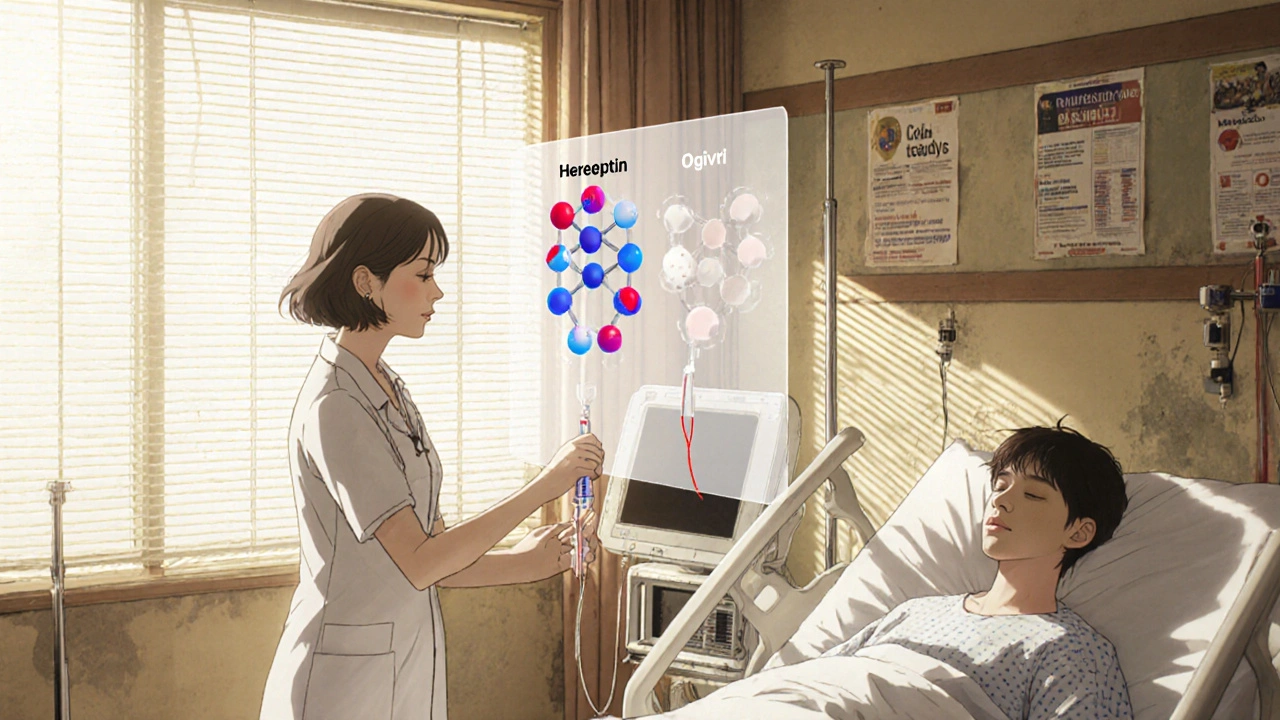
Interchangeability: The Next Big Step
Not all biosimilars are the same. Some are just “biosimilar.” Others are “interchangeable.” That’s a higher bar. To get interchangeable status, a biosimilar must prove that switching back and forth between it and the original drug doesn’t increase risks. It’s like proving you can swap out two different brands of insulin without any trouble. Remsima (infliximab) became the first monoclonal antibody biosimilar to earn this status in July 2023. That means pharmacists can swap it for the brand-name drug without asking the doctor - just like with a generic pill. This is a game-changer. It removes one of the biggest barriers: provider hesitation. Many doctors still worry about switching. But when a biosimilar has interchangeable status, it signals to the whole system: this is safe, reliable, and ready for everyday use.Challenges Still in the Way
Despite the progress, adoption isn’t smooth. Patent lawsuits are common. A 2023 study from UC Hastings found that, on average, each monoclonal antibody biosimilar faces 14.7 patent challenges before it can launch. These lawsuits delay access - sometimes for years. Doctors aren’t always confident either. A 2022 survey by the American Society of Clinical Oncology showed only 58% of oncologists felt “very confident” prescribing biosimilars. That’s not because they’re unsafe - it’s because many weren’t trained on them. Pharmacy benefit managers (PBMs) also play a role. They control which drugs get covered and at what cost. In 2023, 32% of biosimilar launches were blocked or restricted by formulary rules that favored the brand-name drug. And then there’s the fear of immune reactions. While the EMA reported only 12 unexpected immune events in over 1.2 million patient-years of use - a rate equal to the original drugs - that’s still one too many. Monitoring continues.
What’s Next?
The pipeline is full. As of September 2023, the FDA had 37 monoclonal antibody biosimilars in review. Six are targeting pembrolizumab (Keytruda), a top immunotherapy for melanoma and lung cancer. If approved, these could bring down the cost of a drug that runs over $150,000 per year. The EMA is also preparing new guidelines for even more complex drugs: bispecific antibodies and antibody-drug conjugates. These are next-generation biologics that attack cancer in multiple ways. Making biosimilars for these will be harder than ever - but the payoff could be huge. IQVIA projects that by 2027, monoclonal antibody biosimilars will make up 35% of all biologic prescriptions in the U.S. - up from 18% in 2022. Cancer treatments will drive most of that growth, accounting for 62% of the volume.Why This Matters
Monoclonal antibody biosimilars aren’t just cheaper versions of expensive drugs. They’re proof that science can make life-saving treatments more accessible without cutting corners. They’re the result of years of research, hundreds of tests, and regulatory systems built to protect patients - not block competition. For someone with breast cancer, a biosimilar trastuzumab might mean another year of treatment. For a family with Crohn’s disease, it might mean keeping the lights on. For the system, it means billions saved - money that can go to other patients, other treatments, other needs. The science is solid. The data is clear. The barriers are human - not technical. And as more doctors, pharmacists, and patients learn the truth about biosimilars, they’ll become the standard - not the exception.Are monoclonal antibody biosimilars the same as generics?
No. Generics are chemically identical copies of small-molecule drugs, like aspirin or metformin. Biosimilars are highly similar versions of complex biological drugs made from living cells. Monoclonal antibodies are large proteins, so exact copies aren’t possible. Biosimilars must prove no clinically meaningful differences in safety or effectiveness, but they’re not identical.
Can biosimilars cause different side effects than the original drug?
The risk is extremely low. Regulatory agencies require extensive testing to ensure biosimilars match the reference product in safety and side effect profile. In rare cases, minor structural differences - like altered sugar attachments - have triggered immune reactions, but these are no more common than with the original drug. Over 1.2 million patient-years of use show no increase in adverse events.
Which biosimilars are interchangeable with their reference products?
As of 2025, Remsima (infliximab) is the only monoclonal antibody biosimilar with FDA interchangeable status. This means pharmacists can substitute it for the brand-name version without a doctor’s approval. Other biosimilars require a specific prescription. More are expected to gain this status as data accumulates.
Why are biosimilars cheaper if they’re so complex to make?
They’re not cheaper to develop - in fact, biosimilar development costs $100-200 million, compared to $1-5 million for generics. But they’re cheaper to sell because they don’t need the same massive marketing and clinical trials as the original. The original drug company spent billions on R&D and promotion. Biosimilar makers only need to prove similarity, not start from scratch. That’s where the savings come from.
How do I know if my doctor is prescribing a biosimilar?
Ask. Biosimilars have different brand names than the reference product - like Truxima instead of Rituxan, or Ogivri instead of Herceptin. Your prescription or pharmacy label will list the exact name. If you’re unsure, call your pharmacy. You have the right to know what you’re getting - and whether it’s a biosimilar.
Ezequiel adrian
November 26, 2025 AT 13:56Bro this is wild 🤯 I thought biosimilars were just cheap knockoffs until I read this. Now I get why my uncle’s cancer treatment cost half as much after they switched. Science is cool when it doesn’t screw people over.
Amanda Wong
November 27, 2025 AT 08:23Let’s be clear: calling these ‘biosimilars’ is a marketing ploy. The FDA’s ‘no clinically meaningful difference’ standard is a joke. If you can’t prove exact molecular identity, you haven’t proven safety. This is how we get silent immune reactions that show up years later in vulnerable populations.
Stephen Adeyanju
November 27, 2025 AT 18:45So you’re telling me a drug that costs 150k a year can be cut in half just because someone else figured out how to grow the same protein in a different tank
And the pharma companies are still suing them into oblivion
What even is America anymore
Asia Roveda
November 29, 2025 AT 15:33Let me guess - this is one of those ‘biosimilars are great’ articles written by someone who works for a PBM. 32% of launches blocked? That’s because they’re not profitable. And don’t even get me started on how these ‘cost savings’ are siphoned into executive bonuses while patients still ration insulin.
Aaron Whong
November 30, 2025 AT 13:05The ontological gap between small-molecule generics and monoclonal antibody biosimilars is not merely technical - it is epistemological. The reference product is not a static entity but a dynamic, emergent system shaped by cellular microenvironments, post-translational noise, and stochastic glycosylation pathways. To equate biosimilarity with equivalence is to commit a category error rooted in Cartesian reductionism.
What we are witnessing is not drug substitution but the institutionalization of probabilistic therapeutic identity - a paradigm shift in pharmacological ontology that challenges the very notion of ‘sameness’ in medicine.
Deborah Williams
November 30, 2025 AT 19:01It’s funny how we celebrate innovation that lowers costs - until it’s not made by a white male CEO in a lab coat. We’ll praise a biosimilar when it saves a family money, but if it’s made in India or Germany, suddenly it’s ‘not the same.’ The real barrier isn’t science - it’s our stubborn belief that expensive equals better.
And yet, we still trust generic aspirin. Why not generic antibodies?
mohit passi
December 1, 2025 AT 10:39India making biosimilars for the world 🇮🇳❤️
My cousin got trastuzumab biosimilar in Mumbai - same results as US, cost $300 vs $12k
Global health isn’t about patents - it’s about people
👏👏👏
Cynthia Springer
December 2, 2025 AT 00:16How do they even test for glycosylation differences across thousands of batches? Is it just mass spec? Or do they use some kind of functional assay? I’m curious about the actual methods behind the ‘highly similar’ claim.
Marissa Coratti
December 2, 2025 AT 03:04While the statistical data presented in this article is undeniably compelling - particularly the 28% cost reduction observed in the JAMA Oncology cohort study - one must not overlook the broader sociopolitical context in which these biosimilars are being introduced. The pharmaceutical industry’s entrenched intellectual property frameworks, coupled with the systemic inertia of clinical prescribing habits and the profit-driven incentives of pharmacy benefit managers, collectively constitute a formidable barrier to equitable access. Moreover, the psychological phenomenon of ‘brand loyalty’ among both physicians and patients, rooted in cognitive biases such as the familiarity heuristic and the availability cascade, significantly impedes adoption despite robust safety profiles. It is not merely a matter of scientific equivalence - it is a cultural and institutional recalibration that must occur before biosimilars can achieve true mainstream integration.
Rachel Whip
December 3, 2025 AT 16:17Just a heads-up: if you’re on a biosimilar, always check the lot number and report any unusual reactions to your doctor. The FDA’s MedWatch system tracks these, and your report helps improve safety for everyone. Also - your pharmacist can tell you if it’s interchangeable. Don’t be shy to ask.
Micaela Yarman
December 4, 2025 AT 05:40As a healthcare policy researcher from the Midwest, I’ve seen firsthand how biosimilars have transformed rural oncology clinics. A single patient switching from Humira to Hyrimoz doesn’t just save $5,000 - it frees up Medicaid funds to cover three other patients’ mammograms. This isn’t just science. It’s justice.