CKD Medication Dosing Calculator
Medication Selection
When you have both Type 2 Diabetes and Chronic Kidney Disease (CKD), managing your medications isn’t just about lowering blood sugar-it’s about protecting your kidneys and avoiding life-threatening side effects. For years, doctors held off on prescribing metformin if your kidneys weren’t working well. Now, that’s changed. And SGLT2 inhibitors, once seen as only for early-stage CKD, are being used even when kidney function is severely reduced. The rules have been rewritten. If you’re on either of these drugs-or thinking about starting them-here’s what you actually need to know in 2026.
Metformin in CKD: It’s Safer Than You Think
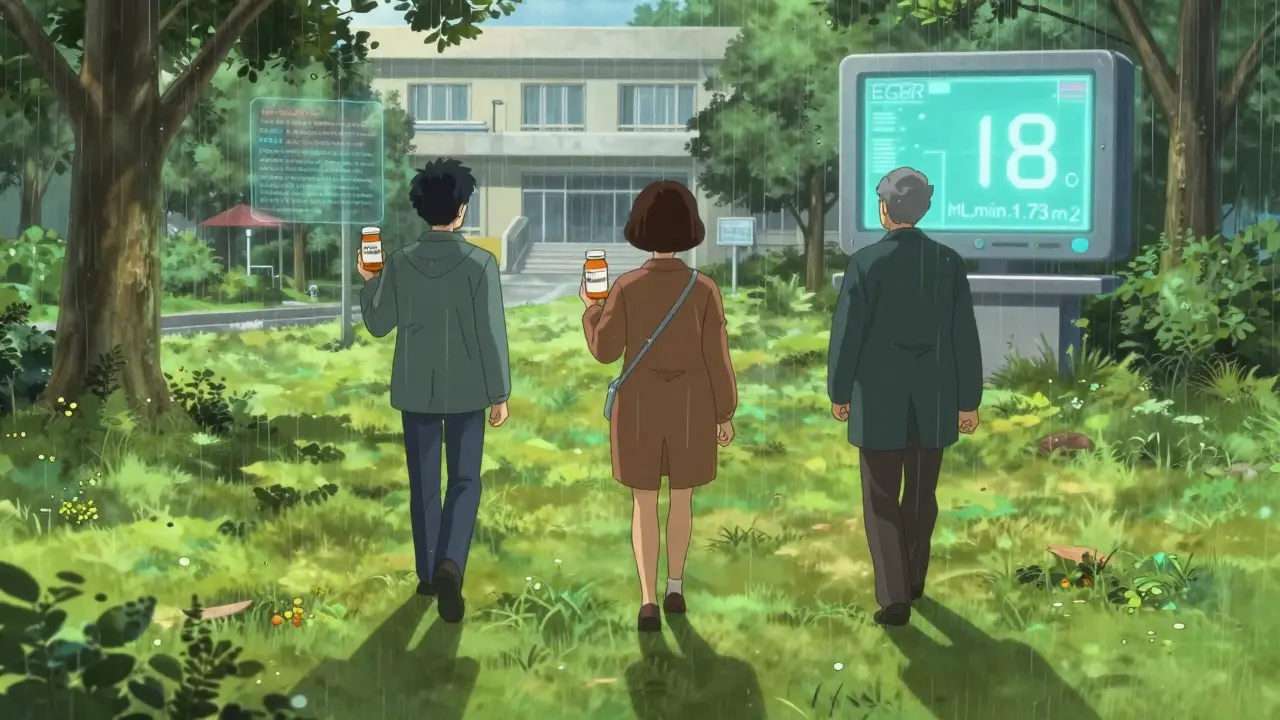
Metformin used to be a no-go if your eGFR dropped below 60. That was the old rule. Today, the guidelines have shifted dramatically. The KDIGO 2022 Clinical Practice Guideline, backed by data from over 28,000 patient-years of research, now says metformin is safe at eGFR levels as low as 30 mL/min/1.73 m². That’s a big deal. Many patients were taken off metformin too early, missing out on its proven benefits: better blood sugar control, weight neutrality, and even a lower risk of heart failure.
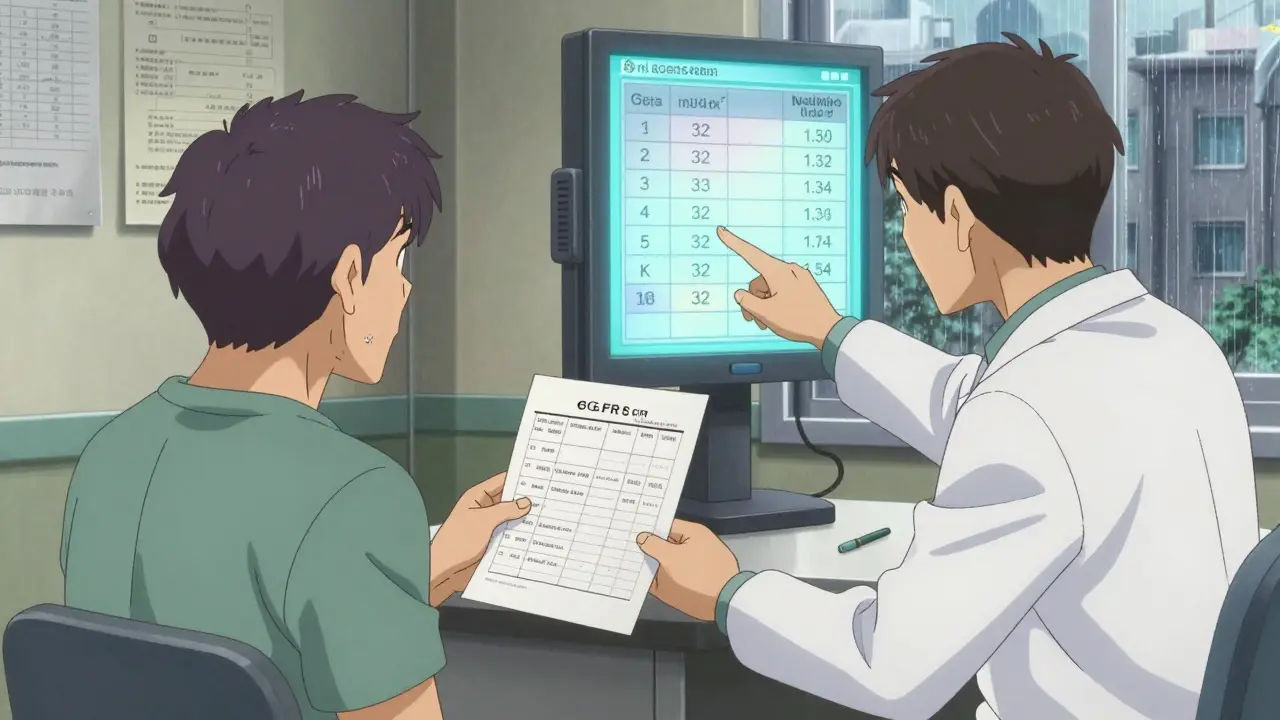
Here’s how dosing works today:
- eGFR ≥60: Standard dose-up to 2,000 mg daily (usually 500-850 mg twice daily).
- eGFR 45-59: Max dose is 1,000 mg daily. Don’t push higher, even if your sugar is still up.
- eGFR 30-44: Max dose stays at 1,000 mg daily. No need to reduce further unless you’re at high risk for lactic acidosis.
- eGFR <30: Stop metformin. Don’t wait for symptoms. This includes patients on dialysis.
Why the change? Because lactic acidosis-the scary side effect everyone feared-is extremely rare when metformin is used correctly. Studies show the risk is only 3-10 cases per 100,000 patient-years in the general population. Even in CKD, it’s under 50 per 100,000 when doses are adjusted. The FDA removed the absolute contraindication in 2016 after reviewing 15 years of data. Now, the real danger isn’t metformin itself-it’s failing to monitor eGFR or continuing the drug during acute kidney injury.
SGLT2 Inhibitors: The New Foundation of CKD Care
If metformin is the old workhorse, SGLT2 inhibitors are the new backbone of treatment. These drugs-dapagliflozin, empagliflozin, canagliflozin, ertugliflozin-don’t just lower blood sugar. They reduce heart failure, slow kidney decline, and cut the risk of death by up to 30% in people with CKD. The evidence is so strong that KDIGO now recommends them as first-line therapy for anyone with Type 2 Diabetes and CKD, regardless of their HbA1c.
Here’s the biggest update: you can now start an SGLT2 inhibitor even if your eGFR is as low as 20 mL/min/1.73 m². Before 2022, the cutoff was 30. That change came from trials like DAPA-CKD and EMPEROR-Preserved, which showed clear benefits even in advanced CKD. In DAPA-CKD, 11% of participants had eGFR between 25-30. They still got protection from kidney failure and heart events.
And here’s something most people don’t realize: once you start an SGLT2 inhibitor, you don’t need to stop it just because your eGFR drops below 20. The KDIGO guideline says you can keep using it-even if you’re on dialysis. That’s based on emerging data from ongoing studies. The lowest effective dose for kidney and heart protection is:
- Dapagliflozin: 10 mg daily
- Empagliflozin: 10 mg daily
- Canagliflozin: 100 mg daily
- Ertugliflozin: 5 mg daily
Higher doses don’t give more kidney protection. They just raise the risk of side effects. Stick to the low dose. That’s all you need.
Safety Risks: What to Watch For
Both drugs are safe when used right-but you still need to know the red flags.
Metformin risks: The main concern is lactic acidosis, but it’s rare. Watch for unexplained fatigue, muscle pain, trouble breathing, or stomach upset-especially if you’re dehydrated, sick, or having surgery. If your eGFR drops suddenly due to infection, heart failure, or dehydration, stop metformin immediately. Don’t wait for lab results. Recheck eGFR in 48 hours before restarting.
SGLT2 inhibitor risks: These are different. The most common issue is genital yeast infections-4-5% of women, 1-2% of men. Keep the area clean and dry. If you’re uncircumcised or postmenopausal, you’re at higher risk. Second, volume depletion. These drugs make you pee more. If you’re elderly, on diuretics, or not drinking enough, you could get dizzy, weak, or have low blood pressure. Drink water. Don’t skip meals. Third, diabetic ketoacidosis (DKA). This is rare-only 0.1-0.2% of users-but it can happen even when blood sugar isn’t high (euglycemic DKA). Symptoms: nausea, vomiting, abdominal pain, confusion. If you’re sick, stop the SGLT2 inhibitor and check for ketones with a urine strip or blood test.
Also, if you’re on finerenone (a newer kidney-protective drug), monitor potassium. Keep it under 5.5 mmol/L. If it spikes, hold finerenone until it drops below 5.0.
Combining Metformin and SGLT2 Inhibitors
This is now the gold standard. KDIGO 2022 says: if you have T2D and CKD with eGFR ≥30, start both drugs together. No need to wait. No need to try other medications first. The combination gives you the best of both: metformin’s glucose control and SGLT2 inhibitors’ heart and kidney protection.
But here’s the catch: if you’re also on insulin or sulfonylureas, you might need to reduce those doses. SGLT2 inhibitors lower blood sugar independently. Add them to a high-dose sulfonylurea, and you risk dangerous lows. The UK Kidney Association recommends:
- Reduce sulfonylurea or meglitinide dose by 50% if HbA1c is below 58 mmol/mol and eGFR >45.
- Reduce insulin dose by 20% under the same conditions.
Don’t guess. Work with your doctor to adjust. A 2022 survey found that 68% of primary care doctors didn’t know how to adjust doses properly. You’re not alone if this feels confusing.
Monitoring: What to Track and When
These drugs aren’t set-and-forget. You need regular checks.
For metformin:
- Check eGFR every 3-6 months if it’s above 45.
- Check every 1-3 months if eGFR is between 30-44.
- Stop immediately if eGFR drops below 30.
For SGLT2 inhibitors:
- Check for genital infections monthly for the first 3 months.
- Monitor blood pressure and signs of dehydration-especially if you’re older or on diuretics.
- Check ketones if you feel unwell, even if your blood sugar is normal.
- Keep eGFR tracked, but don’t stop the drug just because it dips below 20. Keep going unless there’s another reason.
Many patients get dropped from these drugs after a single eGFR dip-often due to dehydration or illness. That’s a mistake. Recheck after recovery. Don’t assume the kidney damage is permanent.
Why So Many Patients Still Aren’t Getting These Drugs
Despite the strong evidence, real-world use is lagging. At Baylor College of Medicine, 37% of patients with eGFR 20-29 weren’t on an SGLT2 inhibitor in early 2023. Why? Doctors were afraid. They were taught the old rules. Many still think “eGFR below 30 = no SGLT2i.”
A 2022 survey of 1,200 primary care doctors found only 34% knew the correct dosing thresholds. After a 60-minute training, that jumped to 78%. The problem isn’t the science-it’s the speed of change. Nephrologists are catching up. Primary care? Not so fast.
And there’s another layer: access. A 2023 JAMA study found SGLT2 inhibitor use in advanced CKD was over three times higher in high-income patients than low-income ones. These drugs are expensive. Insurance coverage varies. If you’re struggling to afford them, ask about patient assistance programs. Generic versions are coming. Empagliflozin’s patent expires in 2026. Prices will drop.
What’s Next? The Future of CKD Treatment
The ZEUS trial (NCT05225191) is now studying dapagliflozin in patients with eGFR as low as 15 mL/min/1.73 m². Results are due in late 2025. Early data from the DAPA-CKD-Extension study suggests SGLT2 inhibitors are safe even on dialysis. One expert predicts they’ll become standard for dialysis patients within five years.
And it’s not just about drugs. The KDIGO Steering Committee plans to update its guideline in Q2 2024, incorporating new data from EMPA-KIDNEY and DELIVER. The message is clear: we’re moving toward earlier, broader, and more aggressive use of kidney-protective therapies.
If you have CKD and diabetes, don’t wait for your doctor to bring it up. Ask: “Am I on the right meds for my kidney health?” If you’re on metformin, ask: “Is my dose still right for my eGFR?” If you’re not on an SGLT2 inhibitor, ask: “Why not?” The science is no longer in question. The question now is: who gets access to what works?
Joanna Brancewicz
January 8, 2026 AT 00:48Metformin at eGFR 30 is a game-changer. I’ve seen patients crash because they were pulled off it too soon-then their HbA1c went through the roof. This isn’t just about kidneys; it’s about quality of life.
Stop treating eGFR like a cliff edge. It’s a slope. And we’re finally climbing it.
Evan Smith
January 9, 2026 AT 11:21So let me get this straight-we’re saying doctors were too scared to use a $5-a-month drug because they didn’t update their 2010 textbook?
Meanwhile, my cousin’s on insulin pumps and still gets DKA because no one told her SGLT2i works even if her kidneys are ‘failing.’
Lois Li
January 10, 2026 AT 19:37I’m a nurse in a rural clinic and this is exactly what we’ve been fighting for. Patients get dropped from SGLT2 inhibitors after one cold, one dehydration episode, and we lose the benefits. We need better education-not just for docs, but for patients too.
Maybe we start with handouts in Spanish, Hindi, and plain English. No jargon. Just: ‘This protects your heart and kidneys. Don’t stop unless your doctor says.’
Ken Porter
January 12, 2026 AT 09:44Of course the guidelines changed. Leftist medical boards don’t care about real outcomes-they care about political correctness.
Metformin causes lactic acidosis. Period. If your kidneys are bad, you shouldn’t be on anything. Let the big pharma companies profit off fear.
swati Thounaojam
January 12, 2026 AT 11:24My uncle in Delhi was taken off metformin at eGFR 48. Now he’s on insulin 3x a day. No one told him about the new rules. India’s healthcare is slow to change. Hope this reaches more docs here.
Luke Crump
January 13, 2026 AT 23:16What if the real issue isn’t the drugs… but the belief that we can ‘fix’ chronic disease with pills?
We’ve turned kidneys into widgets. ‘Adjust dose at eGFR 30.’ Like it’s a car’s oil change.
What about diet? What about sleep? What about the fact that 70% of CKD patients live in poverty?
We’re treating symptoms while the system burns.
Manish Kumar
January 14, 2026 AT 13:24Let me tell you something-this whole metformin thing is a perfect example of how medicine gets hijacked by corporate-funded studies. The KDIGO guidelines? Funded by big pharma. The ZEUS trial? Sponsored by AstraZeneca. The DAPA-CKD study? Eli Lilly’s baby.
Yes, the drugs work. But why is it only now that we’re ‘safe’ at eGFR 30? Why not 5 years ago? Because the data took time to accumulate, sure-but also because the profit model needed to align. Metformin’s generic. SGLT2 inhibitors? $800/month. So they pushed the envelope. And now we’re all supposed to cheer because the safety window got wider?
It’s not progress-it’s rebranding.
Aubrey Mallory
January 14, 2026 AT 18:47Ken, you’re not helping. And Evan, you’re right to be furious-but don’t let anger blind you to the real win here: people are living longer because we’re finally listening to the science.
Yes, access is unequal. Yes, doctors are behind. But we’re moving. And if you’re reading this, you’re part of the change. Ask your doctor. Bring this post. Be the patient who refuses to be ignored.
Dave Old-Wolf
January 15, 2026 AT 08:52My mom’s eGFR is 32. She’s on 500mg metformin twice a day. Last month her creatinine spiked after a UTI. Her PCP wanted to stop everything. I pulled up the KDIGO guidelines, printed them, and took them to her appointment.
She’s still on it. eGFR bounced back to 35 after hydration.
Don’t panic when numbers dip. Recheck. Reassess. Don’t assume it’s permanent.
Also-SGLT2i saved her from heart failure. I didn’t even know that was a possibility until I read this.
Prakash Sharma
January 15, 2026 AT 15:56Why are we even talking about this? In India, most people can’t afford insulin, let alone SGLT2 inhibitors. We need cheap generics NOW. Not guidelines. Not trials. Pills. At ₹50 a month.
Stop celebrating science when people are dying because they can’t buy the medicine.
Donny Airlangga
January 15, 2026 AT 16:15I just want to say thank you to whoever wrote this. My dad’s on dapagliflozin with eGFR 22. They told him he was too far gone. He’s had zero infections, his BP is better, and he walks 2 miles every day now.
This isn’t theoretical. It’s real. And it’s working.
Molly Silvernale
January 16, 2026 AT 02:36They say the kidneys don’t heal-but what if they’re not broken? What if they’re just… tired? Like a battery drained by decades of sugar, stress, and silence?
Metformin isn’t a cure-it’s a whisper. A quiet nudge to the body: ‘Hey, you can still breathe.’
SGLT2 inhibitors? They’re the song that follows.
And maybe-just maybe-we’re finally learning to listen.