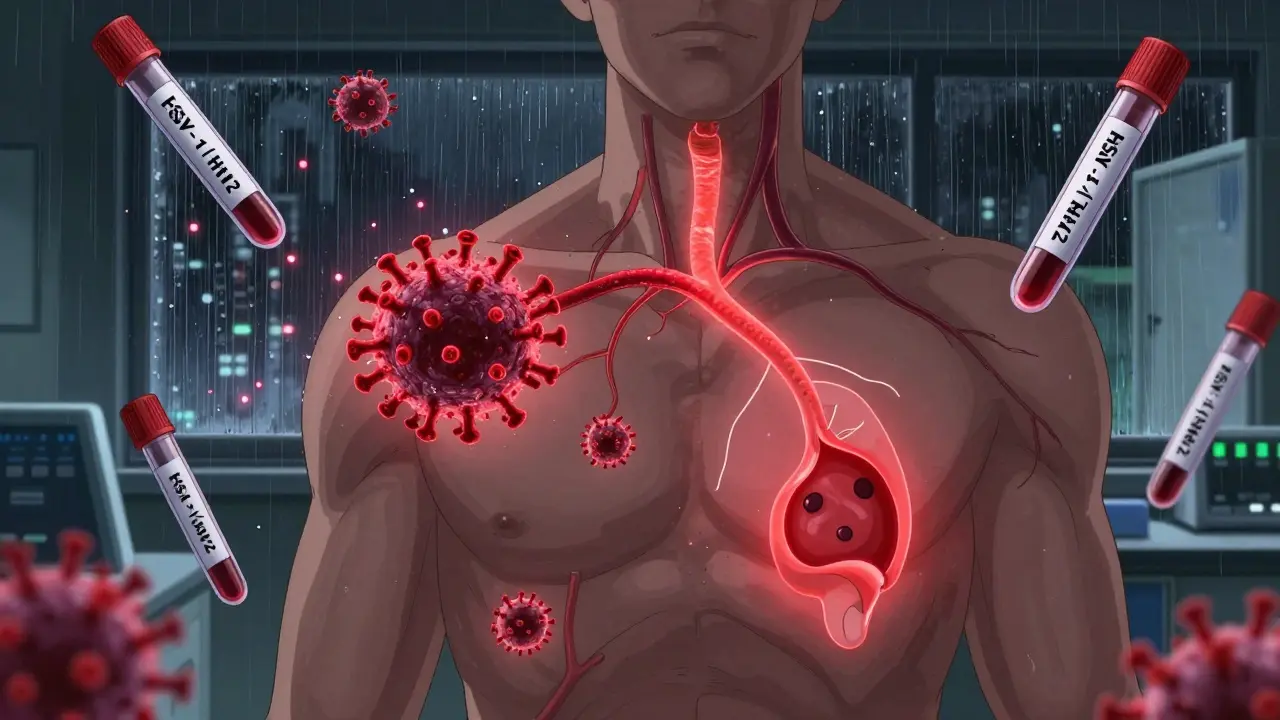
Most people think of cold sores when they hear "herpes." But herpes simplex virus is more than just a lip blister. It’s a lifelong infection that affects billions worldwide - and most don’t even know they have it. There are two types: HSV-1 and HSV-2. They look similar, but their behavior, where they hide in your body, and how they spread are very different. Understanding these differences isn’t just about knowing what a sore looks like - it’s about knowing how to protect yourself, your partner, and even your future children.
What Are HSV-1 and HSV-2? The Real Difference
HSV-1 and HSV-2 are two versions of the same virus family. They share about half their DNA, but that small difference changes everything. HSV-1 was first identified in 1942 and was long thought to only cause cold sores around the mouth. HSV-2, found in 1956, was tied to genital sores. But today, that’s outdated. In high-income countries, HSV-1 now causes 30-50% of new genital infections. Meanwhile, HSV-2 still causes 70-80% of genital outbreaks, but it’s declining in younger populations as safer sex practices spread.
Here’s the key: HSV-1 likes the trigeminal nerve, which runs behind your ear and down to your lips. That’s why it usually shows up as a cold sore. HSV-2 prefers the sacral nerves near your lower spine - which is why it tends to cause genital sores. But both can infect either area. If you get HSV-1 on your genitals, you’re less likely to have repeat outbreaks - about 0.2 to 0.5 times a year. HSV-2? That’s 4 to 5 times a year on average. And while HSV-1 sheds (releases virus without symptoms) on 5-10% of days, HSV-2 sheds on 10-20% of days. That means you can spread HSV-2 even when you feel fine.
What Do the Symptoms Actually Look Like?
Not every infection causes visible sores. In fact, up to 80% of people with HSV-2 never know they’re infected because symptoms are mild or mistaken for something else - like a yeast infection or razor burn. But when symptoms do appear, they follow a pattern.
First, you feel it. A tingling, burning, or itching sensation - often just for a few hours. Then, small red bumps appear. Within a day or two, they turn into fluid-filled blisters, about the size of a pinhead to a pea. These break open, form painful ulcers, then crust over. Healing takes 7 to 21 days for a first outbreak. Recurrent ones? Usually 5 to 10 days.
Primary oral HSV-1 in kids often looks like herpetic gingivostomatitis: fever over 38.5°C, mouth full of ulcers, bad breath, and trouble swallowing. About 5-10% of these kids end up in the hospital because they can’t drink. In adults, it’s usually just one or two cold sores on the lip.
Primary genital HSV-2 is worse. Over 90% of people get painful ulcers. Most also have trouble peeing (dysuria), swollen lymph nodes in the groin, and sometimes vaginal or urethral discharge. About 4 in 10 get a fever and muscle aches. It’s not uncommon for someone to mistake this for a UTI - until they see the sores.
How Is It Diagnosed? Don’t Rely on Guesswork
Doctors used to swab sores and wait days for a culture. Now, PCR testing is standard. It detects the virus’s DNA and is 95-98% accurate. Results come back in 24 to 72 hours. If you don’t have active sores, a blood test can tell you if you’ve been exposed. Type-specific tests like HerpeSelect or EUROIMMUN’s recomLine HSV IgG look for antibodies to HSV-1 or HSV-2. These are 97-98% accurate if taken 16 weeks after possible exposure. Earlier tests can give false negatives.
Don’t get tested too soon. If you had a risky encounter two weeks ago and get a blood test, it might say negative - even if you’re infected. Your body needs time to make antibodies. Wait. And if you have symptoms, get a swab done right away. The sooner you test, the better your treatment window.
Antiviral Therapy: What Actually Works
There’s no cure - but there are three antiviral drugs that control it: acyclovir, valacyclovir, and famciclovir. They don’t kill the virus. They stop it from copying itself. That’s enough to shorten outbreaks, reduce pain, and lower how often you spread it.
For a first outbreak, the CDC recommends acyclovir 400mg three times daily for 5-10 days. Valacyclovir (500mg twice daily) or famciclovir (250mg three times daily) work just as well and are easier to take. These drugs cut healing time from 19 days to about 10. Pain drops from 12 days to 8.
If you get outbreaks more than six times a year, daily suppressive therapy helps. Valacyclovir 500mg once a day reduces transmission to partners by 48%. For HSV-1 genital infections, this isn’t always needed - only 25% of people have more than one outbreak a year. But for HSV-2, it’s a game-changer.
For eye infections (herpes keratitis), topical trifluridine drops are used hourly. For brain infections (herpes encephalitis), high-dose IV acyclovir (10mg/kg every 8 hours) is critical. Delayed treatment increases death risk.
What About Resistance and New Treatments?
Most people respond well. But in those with weakened immune systems - like people with HIV and CD4 counts under 100 - up to 10% of HSV strains resist acyclovir. When that happens, doctors switch to foscarnet or the newer drug pritelivir. In March 2023, the FDA approved pritelivir for acyclovir-resistant HSV. It cuts viral shedding by 87% in 48 hours - far better than older options.
There are also vaccines in trials. GEN-003 and Simplirix showed 50% less viral shedding in early studies. But none are approved yet. For now, antivirals remain the gold standard. New drugs like amenamevir (used in Japan) are being studied too. They work faster - suppressing the virus in 24 hours versus 60% for acyclovir.

Living With HSV: The Emotional Side
Physical symptoms fade. The stigma doesn’t always. A 2023 survey by the American Sexual Health Association found 74% of people with HSV feel anxiety about stigma. 45% say it’s hurt their relationships. One in three waited over six months to tell a partner.
But real stories tell a different truth. On Reddit, users report that after the first outbreak - often terrifying - daily valacyclovir turns HSV from a crisis into a manageable condition. One user wrote: "First outbreak lasted 18 days with fever and 12 ulcers. Now, with daily meds, I get 2-3 days of one tiny lesion, maybe twice a year. I’m not hiding anymore."
Side effects from antivirals are rare. Headache and nausea happen in 15-22% of users. Kidney issues are only a concern if you already have kidney disease. Switching from acyclovir to famciclovir often solves nausea problems.
Cost is a barrier. Valacyclovir 500mg costs $35-60/month with insurance. Without, it’s $300-400. Generic acyclovir is cheaper - $10-20/month. Many clinics offer patient assistance programs.
What You Can Do Right Now
- If you have a first outbreak, see a doctor within 24 hours. Treatment started early cuts healing time in half.
- If you have frequent outbreaks, ask about daily suppressive therapy. It reduces transmission and improves quality of life.
- If you’re pregnant and have HSV, tell your OB-GYN. If you have an outbreak near delivery, a C-section reduces neonatal herpes risk from 30-50% to 1-3%.
- If you’re in a relationship with someone who has HSV, use condoms and consider suppressive therapy. Transmission risk drops by nearly half.
- Don’t rely on symptoms alone. You can spread HSV without sores. Testing is the only way to know for sure.
Herpes isn’t a death sentence. It’s a chronic condition - like high blood pressure or diabetes. You manage it. You don’t let it define you. The science is clear. The tools exist. What matters now is knowing how to use them.
Can you get herpes from sharing a towel or toilet seat?
No. Herpes simplex virus doesn’t survive long outside the body. It needs direct skin-to-skin contact with an infected area - usually during an outbreak or asymptomatic shedding. You can’t catch it from towels, toilet seats, or swimming pools.
Is herpes only spread through sex?
No. HSV-1 is often spread through kissing, sharing utensils, or touching a cold sore and then touching your genitals. That’s why more young people are getting genital HSV-1 - not from sex, but from oral contact. HSV-2 is mainly spread through sexual contact, but skin-to-skin contact without penetration can still transmit it.
Can you have kids if you have herpes?
Yes. Most women with herpes have healthy babies. The risk comes if you have an active outbreak during delivery. If you’ve had herpes before and aren’t having an outbreak, the risk of passing it to your baby is less than 1%. If you have a first outbreak late in pregnancy, your doctor will likely recommend a C-section to reduce the risk from 30-50% down to 1-3%.
Do antivirals cure herpes?
No. Antivirals like acyclovir and valacyclovir don’t eliminate the virus. They suppress it. Once infected, the virus stays in your nerves for life. But with daily treatment, many people have no outbreaks at all - or only one every few years. You can live a normal, healthy life without passing it on.
How do I know if I have HSV-1 or HSV-2?
You need a type-specific blood test or a PCR swab from an active sore. Symptoms alone can’t tell you. HSV-1 can cause genital sores, and HSV-2 can cause cold sores. Only lab testing confirms which type you have. This matters because HSV-2 recurs more often and sheds more frequently.
Can I still have sex if I have herpes?
Yes - but be honest and take precautions. Use condoms, avoid sex during outbreaks, and consider daily suppressive therapy. These steps reduce transmission risk by 70% or more. Many couples where one partner has HSV and the other doesn’t stay together for decades without transmission.
What Comes Next?
Herpes is common. It’s manageable. It’s not shameful. The real danger isn’t the virus - it’s the silence around it. More people need to get tested. More people need to know how antivirals work. And more people need to stop believing myths.
If you’ve been diagnosed, you’re not alone. Over 3.7 billion people have HSV-1. Nearly half a billion have HSV-2. The tools to live well with it exist. Use them. Talk to your doctor. Ask about testing, treatment, and prevention. Your health - and your relationships - depend on it.
sagar sanadi
January 20, 2026 AT 09:53clifford hoang
January 21, 2026 AT 00:14Thomas Varner
January 22, 2026 AT 09:06Art Gar
January 22, 2026 AT 15:55Shane McGriff
January 24, 2026 AT 09:33Carolyn Rose Meszaros
January 25, 2026 AT 11:35Jacob Cathro
January 27, 2026 AT 05:56Greg Robertson
January 28, 2026 AT 19:47Nadia Watson
January 30, 2026 AT 08:12pragya mishra
January 30, 2026 AT 17:25Manoj Kumar Billigunta
January 31, 2026 AT 17:19kumar kc
February 2, 2026 AT 01:43Andy Thompson
February 2, 2026 AT 13:18Edith Brederode
February 4, 2026 AT 12:05Paul Barnes
February 5, 2026 AT 21:51