Side Effect Trade-Off Calculator
Understand Side Effects in Real Terms
Instead of saying "15% chance," ask: "15 out of 100 people experience this." This calculator shows how side effects translate to real people. Use it to prepare questions for your next appointment.
Use this in your next appointment:
- Ask: "How many people out of 100 experience this?"
- Ask: "Which side effect would be a deal-breaker for you?"
- Ask: "How would this affect your daily life?"
Why This Matters
Shared decision-making is about understanding real impacts, not just percentages.
Patients who discuss side effect trade-offs using absolute numbers are:
- 29% less likely to quit treatment due to unexpected side effects
- 22% fewer follow-up visits for side effect concerns
- 33% less likely to discontinue statins due to muscle pain
When you’re told you need a new medication, the conversation often goes like this: "This will help your blood pressure, but you might get dizzy or feel tired." That’s it. No numbers. No real talk about what matters to you. And yet, millions of people stop taking their meds because the side effects feel worse than the disease. The problem isn’t the medicine-it’s the conversation.
Why Side Effect Trade-Offs Are Hard to Talk About
Most doctors mean well. They want to help. But when they say "rare side effect" or "some people feel nauseous," they’re leaving you guessing. Is "rare" one in a hundred? One in ten? And what does "feeling nauseous" really mean? Will it ruin your mornings? Keep you from work? Make you skip meals? The truth is, side effects aren’t just medical facts-they’re life disruptions. A 2022 study at Scripps Health found that 42% of patients who regretted starting a long-term medication didn’t regret the illness. They regretted how the treatment changed their daily life. That’s why simple consent forms don’t cut it anymore. You need a real conversation.The SHARE Approach: A Step-by-Step Framework
The Agency for Healthcare Research and Quality (AHRQ) created the SHARE Approach to fix this. It’s not a script you memorize. It’s a way of thinking. Here’s how it works in practice:- Seek opportunities - Start by asking: "Are you open to talking about how this treatment might affect your day-to-day life?" This gives permission. It’s not about pushing a decision-it’s about inviting input.
- Help explore options - Don’t just say "take this pill." Say: "You have two choices. One reduces your stroke risk by 30%, but 1 in 10 people get bad nausea. The other has less nausea-only 1 in 20-but it’s 15% less effective at preventing strokes. Which trade-off feels more manageable to you?"
- Assess values - This is the key. Ask: "What side effects would make you say no to this treatment?" Some people can live with mild fatigue. Others can’t stand even a 10% chance of dizziness. There’s no right answer. Only what matters to you.
- Reach a decision - Don’t assume you’ve agreed. Say: "So, if we pick Option A, you’re okay with the nausea because you really want to avoid the stroke risk?" Then pause. Let them say yes, or correct you.
- Evaluate - Check in later. "How’s the nausea been? Are you still happy with this choice?" This isn’t a one-time talk. It’s a relationship.
The Three-Talk Model: Numbers That Stick
The three-talk model adds precision. It’s used heavily in oncology and cardiology because it cuts through fear and confusion. Here’s how it works:- Option talk - Present options with numbers. Say: "This drug causes nausea in 15 out of 100 people. That means 85 out of 100 don’t have it." Never say "common" or "rare." Those words mean nothing.
- Preference talk - Ask: "Which side effect would be a deal-breaker for you?" One patient said, "I’d rather have a stroke than throw up every morning." That’s not irrational. That’s a life choice.
- Decision talk - Summarize: "So you’re choosing the higher-risk option because you’re okay with nausea, but you can’t risk missing work. Is that right?" Then write it down.
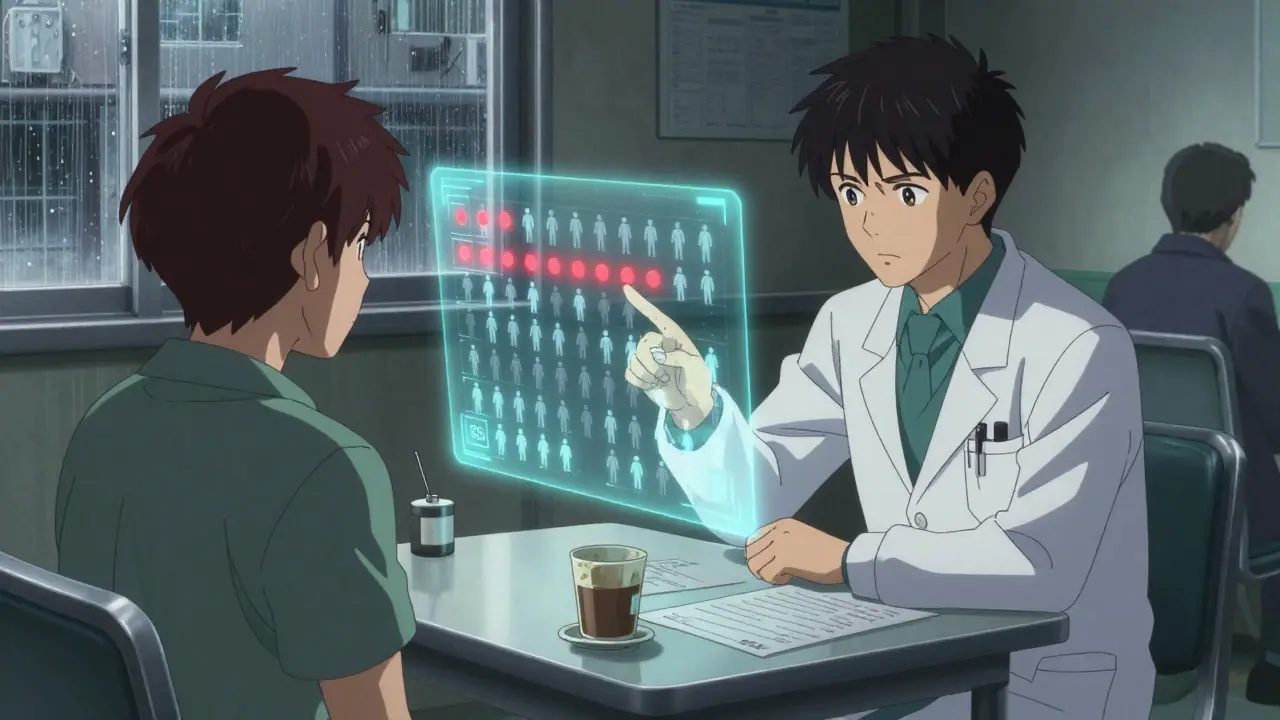
Research from the Annals of Internal Medicine shows patients understand risk 37% better when you use absolute numbers-like "15 out of 100"-instead of percentages like "15% chance." Why? Because our brains don’t do abstract math. We think in people.
What Works in Real Life
A 2021 trial in JAMA Internal Medicine followed patients on chemotherapy. Those who had structured SDM conversations were 29% less likely to quit treatment because of side effects they didn’t expect. That’s not magic. That’s clarity. At Kaiser Permanente, they started giving patients a 5-minute video before appointments explaining statin side effects using visuals: a bar chart showing 86 out of 100 people have no muscle pain, 14 do. Then, in the visit, the doctor asked: "Would 14% muscle pain be too much for your daily walks?" Result? Statin discontinuation dropped by 33%. And it’s not just about pills. For anticoagulants, where major bleeding affects 3-5% of users yearly, patients who used SDM scripts were 23% less likely to feel decisional conflict. They knew their risk. They chose it. And they stuck with it.
What Doesn’t Work
Scripts fail when they feel robotic. A 2022 survey found that 63% of patients felt frustrated when doctors "read from a list" without listening. One patient wrote: "He asked me what side effects I feared. Then he didn’t even look up from his screen. He just checked a box. I felt like a checkbox, not a person." The same study showed that when clinicians used rigid scripts without adapting, patient satisfaction dropped by 19%. That’s the danger. Structure helps. Automation hurts.Visual Aids Make a Difference
Color-coded charts. Risk thermometers. Icons showing how many people experience each side effect. These aren’t gimmicks. They’re tools. Scripps Health found that when doctors used simple visuals during SDM conversations, patient satisfaction jumped by 41%. Why? Because seeing 15 red dots out of 100 makes the risk real. Numbers on paper? They blur.Time Is the Biggest Hurdle
Yes, doing this right takes time. Studies show an extra 7.3 minutes per visit. That’s a lot in a busy clinic. But here’s the flip side: those same patients had 22% fewer follow-up visits for side effect complaints. That’s time saved later. The solution? Pre-visit materials. A short video. A one-page handout. Something that gives patients time to think before the appointment. That cuts the conversation time by over 3 minutes. It’s not about doing more in the room. It’s about doing it better.
It’s Not Just for Chronic Illness
You might think this only matters for statins or blood thinners. But it matters for antibiotics, antidepressants, even pain meds. A 2023 study on painkillers showed that patients who discussed side effect trade-offs were far more likely to stick with the treatment-even if they got mild drowsiness-because they’d chosen it, not just accepted it.What’s Changing Now
In 2023, Medicare Advantage plans had to start documenting shared decision-making for high-risk drugs. That’s not a suggestion. It’s a rule. And it’s driving adoption. Epic’s electronic health record system now includes built-in SDM modules for common conditions-diabetes, heart disease, depression-with pre-loaded scripts and risk charts. The American Medical Association even created new billing codes (96170-96171) to reimburse doctors $45-$65 for documented SDM visits. That’s recognition. That’s legitimacy.What You Can Do
If you’re the patient:- Ask: "What side effects are most likely to affect my daily life?"
- Ask: "What’s the chance of that happening?" Then ask for numbers: "Out of 100 people?"
- Ask: "Which side effect would make you stop this treatment?"
- Ask: "Can I have a visual or handout to take home?"
If you’re the provider:
- Don’t say "rare." Say "1 in 20."
- Don’t assume. Ask: "What’s your biggest worry?"
- Use a simple chart-even a hand-drawn one.
- Write down what the patient says matters most. Not just "side effects tolerated," but what they called it.
Final Thought: It’s Not About Perfect Consent. It’s About Personal Choice.
The goal isn’t to make everyone agree with the doctor. The goal is to make sure the patient leaves knowing: This is my choice, not just my prescription.Side effects aren’t just risks on a page. They’re missed school pickups. Lost sleep. Cancelled plans. Forgotten hobbies. When you talk about them like they matter to the person-not just the patient-you don’t just improve adherence. You restore dignity.
What’s the difference between informed consent and shared decision-making?
Informed consent is when a doctor tells you the risks and you say "yes." Shared decision-making is when you and your doctor talk through what matters to you-your lifestyle, fears, priorities-and pick a path together. One is a signature. The other is a conversation.
Are side effect trade-offs only important for older patients?
No. People of all ages care about side effects, but differently. A young parent might refuse a medication that causes drowsiness because they can’t afford to miss school pickups. A retiree might accept nausea if it means avoiding hospital visits. Age doesn’t determine risk tolerance-life context does.
Can I use shared decision-making for over-the-counter meds?
Absolutely. Even something like ibuprofen has risks-stomach bleeding, kidney strain. If you’re taking it daily, you should know the trade-offs. Talk to your pharmacist or doctor: "I’m using this every day. What’s the real risk?" That’s shared decision-making in action.
What if I don’t know what side effects to worry about?
That’s normal. Your doctor can help. Ask: "What side effects do most people find most disruptive?" Or: "Which ones make people stop taking the medicine?" That’s often the most useful insight. You don’t need to know everything-just what matters to your life.
Is shared decision-making just for doctors?
No. Pharmacists, nurses, and even health coaches can use these tools. Many clinics now train all staff in basic SDM. You don’t need to be a specialist to ask: "What’s your biggest concern about this treatment?" That simple question changes everything.
Wesley Pereira
January 6, 2026 AT 08:39Isaac Jules
January 7, 2026 AT 14:10Amy Le
January 8, 2026 AT 22:35Ryan Barr
January 9, 2026 AT 02:50Dana Termini
January 10, 2026 AT 03:22Tom Swinton
January 11, 2026 AT 15:23Molly McLane
January 11, 2026 AT 17:45Beth Templeton
January 12, 2026 AT 12:02Cam Jane
January 12, 2026 AT 16:45Pavan Vora
January 13, 2026 AT 04:19Stuart Shield
January 13, 2026 AT 15:06Indra Triawan
January 14, 2026 AT 02:56Susan Arlene
January 15, 2026 AT 00:14Ashley S
January 16, 2026 AT 06:10