Stress-Psoriasis Impact Calculator
How might your stress management techniques improve your psoriasis? This calculator estimates potential reduction based on clinical evidence from the article.
Your Stress Management Plan
Estimated Psoriasis Improvement
Based on your selected techniques and stress level, you could experience:
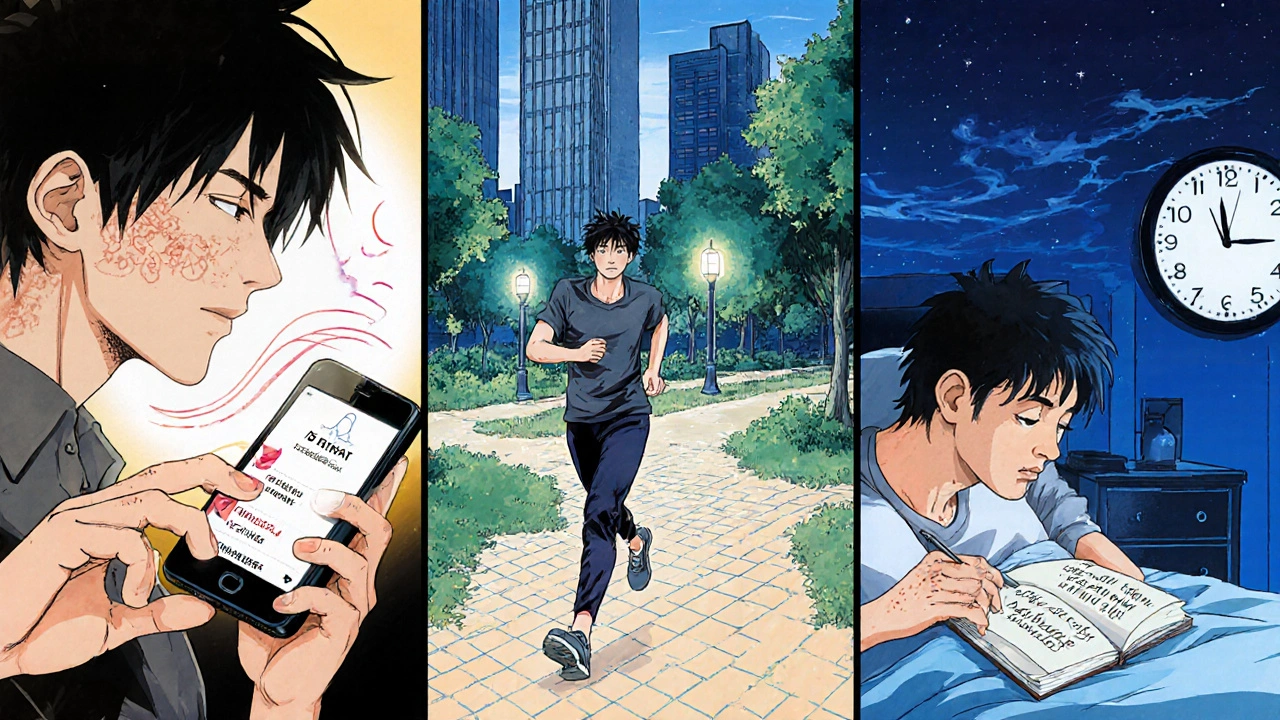
When a skin flare appears out of the blue, many people wonder why. One of the biggest, yet often overlooked, culprits is stress and psoriasis. Understanding how emotional and physical pressure fuels those red, itchy patches can turn frustration into action. Below we break down the science, point out real‑world warning signs, and give you a toolbox of proven techniques to keep stress from stealing your skin’s calm.
How Stress Triggers Psoriasis Flare‑Ups
Psoriasis is an autoimmune skin condition where the immune system mistakenly attacks healthy skin cells, causing them to multiply too quickly. The result? Thick, scaly plaques that can appear anywhere on the body. While genetics set the stage, stress acts like the spotlight that brings the drama to life. When you’re under pressure-whether from work deadlines, relationship tension, or even a lack of sleep-your body releases stress hormones such as cortisol and adrenaline. These chemicals turbo‑charge inflammation, which directly feeds the overactive immune response that drives psoriasis.
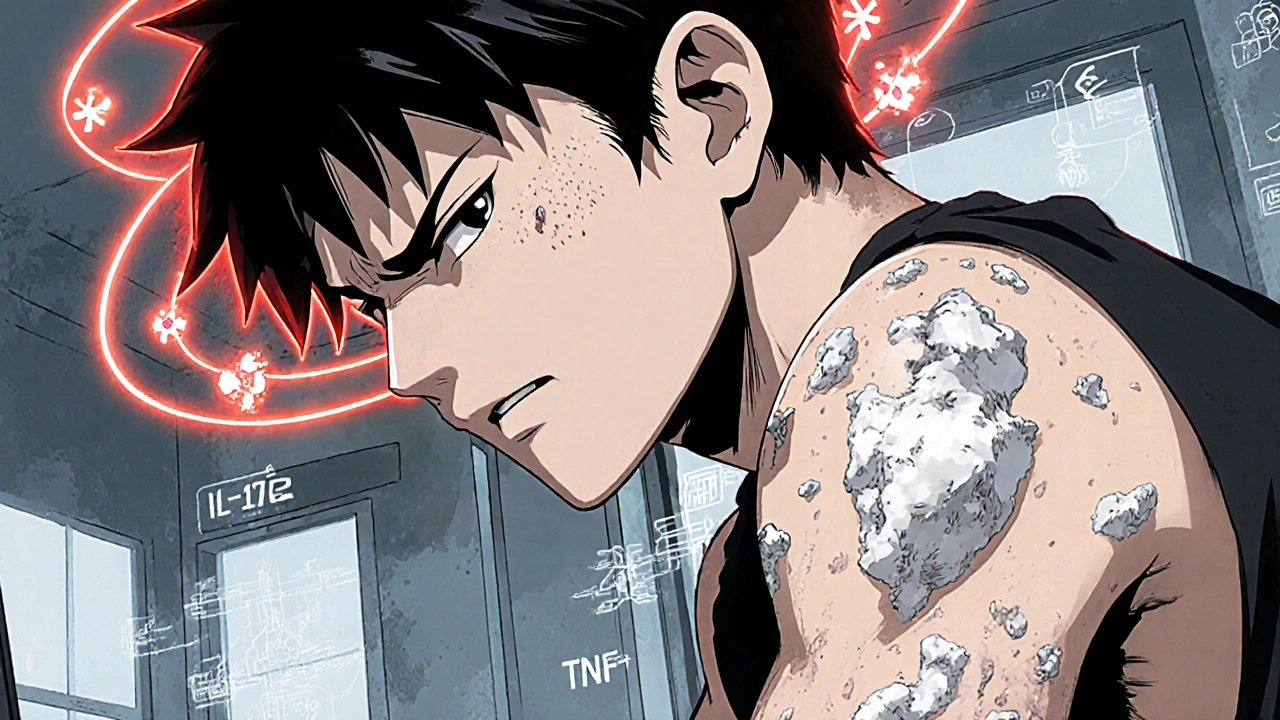
The Biology: Cortisol, Immune Response, and Skin Cells
Stress isn’t just a feeling; it’s a cascade of biochemical events. Cortisol, the primary “stress hormone,” normally helps regulate metabolism and keep inflammation in check. However, chronic elevation of cortisol has a paradoxical effect: it can desensitize the body’s cortisol receptors, making the regulation system less effective. This leads to a spike in pro‑inflammatory cytokines like IL‑17 and TNF‑α, both of which are key players in psoriasis lesions. In short, sustained stress pushes your immune system into a hyper‑reactive mode, and your skin bears the brunt.
Spotting Stress‑Related Triggers in Your Daily Life
Before you can tame the stress‑psoriasis cycle, you need to catch the early warning signs. Keep a simple diary for two weeks and note the following:
- Times when you feel unusually tense or anxious.
- Any new or worsening skin patches that appear within 24‑48 hours after a stressful event.
- Lifestyle factors that often accompany stress-late‑night screen time, caffeine spikes, or skipped meals.
Patterns emerge quickly. For many, a high‑pressure meeting or a heated argument precedes a flare. Recognizing the link empowers you to intervene before the rash spreads.

Proven Strategies to Lower Stress and Calm Your Skin
Below are evidence‑backed approaches that target stress at its source while simultaneously soothing psoriasis.
Mindfulness & Meditation
Multiple clinical trials show that an eight‑week mindfulness‑based stress reduction (MBSR) program can reduce psoriasis severity scores by up to 20%. The practice centers on breathing, body scans, and non‑judgmental awareness, which lowers cortisol levels and improves emotional resilience. Start with just five minutes a day using a free app, and gradually extend to 20 minutes as you get comfortable.
Cognitive‑Behavioral Therapy (CBT)
CBT helps you reframe negative thought patterns that fuel anxiety. A 2023 study of 150 participants found that weekly CBT sessions for three months resulted in a significant drop in both perceived stress and Psoriasis Area and Severity Index (PASI) scores. If you can’t access a therapist in person, many reputable online platforms offer CBT modules tailored for chronic skin conditions.
Physical Activity
Exercise is a natural cortisol regulator. Moderate aerobic activity-like brisk walking, cycling, or swimming-for 30 minutes most days of the week not only cuts stress hormones but also improves circulation, delivering nutrients to skin cells. Resistance training twice a week adds muscle strength, which can further stabilize blood sugar and reduce inflammation.
Sleep Hygiene
Sleep deprivation spikes cortisol and impairs immune balance. Aim for 7‑9 hours of uninterrupted sleep. Create a wind‑down routine: dim the lights an hour before bed, avoid screens, and keep the bedroom cool (around 18‑19 °C). If insomnia persists, consider a short course of melatonin under medical guidance.
Nutrition Adjustments
Certain foods can either aggravate or calm inflammation. Incorporate omega‑3‑rich options-salmon, chia seeds, walnuts-to lower cytokine production. Reduce intake of processed sugars and saturated fats, which are known to worsen both stress and psoriasis. Some patients report benefit from a low‑gluten or Mediterranean‑style diet, but always discuss major changes with a dietitian.
Quick‑Start Checklist for Daily Stress Control
- Morning: 5‑minute guided breath‑focus meditation.
- Mid‑day: 10‑minute brisk walk or stretch break.
- Lunch: Include a serving of oily fish or a handful of nuts.
- Afternoon: Log any stressful moments and rate your skin’s condition.
- Evening: Power‑down screens 60 minutes before bedtime; stretch or do yoga for 15 minutes.
- Night: Write down three things you’re grateful for; set a consistent bedtime.
Follow this routine for at least two weeks. Most people notice reduced itching and fewer new plaques, even if the flare‑ups were previously frequent.
When Stress Management Isn’t Enough: Medical Options
While lifestyle changes are powerful, some cases require medical intervention. If your PASI score stays above moderate despite consistent stress‑reduction efforts, discuss the following options with your dermatologist:
- Topical steroids - quickly calm inflammation for acute patches.
- Vitamin D analogues - help normalize skin cell growth.
- Phototherapy - controlled UV exposure can reset immune activity.
- Biologic therapies - target specific cytokines (e.g., IL‑17 inhibitors) for severe disease.
These treatments work best when paired with stress‑reduction practices, creating a synergistic effect that keeps both the mind and skin in balance.
Comparison of Common Stress‑Management Techniques
| Technique | Effectiveness (PASI reduction) | Typical Time Commitment | Average Cost |
|---|---|---|---|
| Mindfulness Meditation | ~15‑20% reduction | 5‑20 min daily | Free‑to‑low (apps) |
| Cognitive‑Behavioral Therapy | ~20‑25% reduction | 1 hr weekly | Moderate (AU$80‑120 per session) |
| Regular Exercise | ~10‑15% reduction | 30 min most days | Low (no‑equipment) |
| Sleep Optimization | ~5‑10% reduction | Ongoing habit | Low (environment tweaks) |
| Dietary Changes | ~10‑12% reduction | Daily meal planning | Variable (nutrient‑rich foods) |
Frequently Asked Questions
Can stress really cause a psoriasis flare, or is it just a coincidence?
Yes, stress can trigger flares. Scientific studies link elevated cortisol and inflammatory cytokines to worsening psoriasis. While genetics set the baseline, stress often determines when and how severely the disease manifests.
How quickly can I expect to see skin improvement after starting stress‑reduction techniques?
Most people notice a reduction in itching and new plaque formation within 2‑4 weeks of consistent practice. Full visible improvement in existing plaques may take 6‑8 weeks, especially when combined with topical treatment.
Is meditation safe for everyone, including children with psoriasis?
Meditation is generally safe for all ages. For kids, short guided visualizations or breathing games work well. Always keep sessions age‑appropriate and fun to maintain engagement.
Should I stop my prescribed medication while I focus on stress management?
Never stop a prescribed drug without consulting your dermatologist. Stress‑relief methods are complementary; they work best when layered on top of medical therapy.
What role does diet play in the stress‑psoriasis connection?
A diet rich in omega‑3 fatty acids, antioxidants, and low in refined sugars can lower systemic inflammation, which in turn dampens both stress responses and skin flare‑ups. While diet alone won’t cure psoriasis, it supports overall management.
Tammy Sinz
October 22, 2025 AT 20:46From a neuroimmunological perspective, chronic psychosocial stress instigates hyperactivation of the hypothalamic‑pituitary‑adrenal (HPA) axis, leading to sustained cortisol secretion that paradoxically desensitizes glucocorticoid receptors and amplifies pro‑inflammatory cytokine cascades such as IL‑17, IL‑23, and TNF‑α. This mechanistic cascade directly fuels keratinocyte hyperproliferation and the plaque formation characteristic of psoriasis. Moreover, elevated catecholamines during acute stress episodes promote vascular permeability, exacerbating erythema and pruritus. The evidence is unequivocal: stress is not merely a peripheral factor but a central modulator of disease severity. Therefore, integrating rigorous stress‑reduction protocols into standard therapeutic regimens is indispensable for achieving durable remission.
Christa Wilson
October 24, 2025 AT 14:26Absolutely love the practical checklist! 😊 It’s so easy to slip into old habits, but having those bite‑size steps makes it feel doable. Keep spreading the positivity! 🌟
John Connolly
October 26, 2025 AT 07:06Great summary of the stress‑psoriasis link; let me expand on a few points that can help anyone tackling this condition.
First, you’ll want to monitor your cortisol rhythm with a simple salivary test; it’s inexpensive and can reveal hidden spikes.
Second, consider integrating a short, high‑intensity interval training (HIIT) session twice a week; studies show HIIT can blunt cortisol spikes more effectively than moderate cardio.
Third, don’t underestimate the power of breathing exercises – box breathing for five minutes before bed can lower nocturnal cortisol by up to 30%.
Fourth, omega‑3 supplementation should be taken with a meal containing fat to improve absorption, ideally 1–2 grams daily.
Fifth, if you’re sensitive to gluten, trial a strict gluten‑free diet for six weeks and log any skin changes; many patients report noticeable improvement.
Sixth, stay hydrated – aim for at least 2 liters of water per day; dehydration can increase systemic inflammation.
Seventh, keep your environment low‑stress: dim lights, soothing scents like lavender, and minimal noise can reduce sympathetic arousal.
Eighth, use a fragrance‑free moisturizer within five minutes of showering to lock in moisture and support barrier repair.
Ninth, if you’re on biologics, ask your dermatologist about timing your stress‑management practices around dosing to maximize efficacy.
Tenth, consider a digital detox weekend once a month; reducing screen time can improve sleep quality, which in turn stabilizes cortisol.
Eleventh, keep a gratitude journal – focusing on positive experiences can shift autonomic balance toward parasympathetic dominance.
Twelfth, don’t forget regular skin checks; early intervention at the sign of a new flare can prevent larger outbreaks.
Thirteenth, if you notice persistent flares despite these steps, discuss a possible adjustment in medication dosage with your doctor.
Fourteenth, stay connected with supportive communities; shared experiences reduce perceived stress and provide practical tips.
Fifteenth, remember that consistency beats intensity – a daily routine of modest practices outperforms occasional extreme measures.
Sixteenth, celebrate small victories; each week of fewer itch episodes is a win for your skin and mental health.
Sajeev Menon
October 28, 2025 AT 00:46I totally agree with the checklist, but i would add that sometimes a simple cup of chai with ginger can calm both the mind and skin – just make sure it’s not too sugary!
Joe Waldron
October 29, 2025 AT 18:26Here’s a quick rundown: track stressors, note skin changes, prioritize sleep-yes, the usual, but also, try a daily 5‑minute mindfulness break, it’s surprisingly effective; incorporate regular movement, even a short walk works wonders; maintain a balanced diet rich in omega‑3s; stay hydrated, avoid excess caffeine, and don’t forget to keep your dermatologist in the loop.
Sameer Khan
October 31, 2025 AT 12:06When we examine the epistemological underpinnings of psychosomatic interplay, it becomes clear that stress functions as a vector of systemic dysregulation, precipitating immunological perturbations that manifest cutaneously. In this context, therapeutic praxis must adopt a holist paradigm, integrating somatic regulation with pharmacologic modulation to achieve homeostatic equilibrium.
Vin Alls
November 2, 2025 AT 05:46Think of your skin like a canvas; stress throws splatters of anxiety everywhere, but with the right brushstrokes-mindfulness, movement, and a splash of omega‑rich paint-you can turn chaos into a masterpiece. 🎨
Tiffany Davis
November 3, 2025 AT 23:26Consistency is key.
Don Goodman-Wilson
November 5, 2025 AT 17:06Oh great, another self‑help list. Because obviously, the solution to an autoimmune disease is just to breathe deeper and drink some fish oil, right? 🙄
Bret Toadabush
November 7, 2025 AT 10:46Did you know the whole "stress triggers psoriasis" narrative is a smokescreen? Big pharma wants you to buy the newest med while they hide the real cause – the micro‑chips they’ve been implanting since 2015. Wake up!