Reading a prescription label isn’t just about knowing how much to take or when. For people with allergies, it’s a matter of safety. Unlike food, where allergens are clearly listed under federal law, medicine labels don’t follow the same rules. That gap can be dangerous. You might think, "I’ve taken this pill before, it’s fine," but the inactive ingredients could have changed. And those changes? They’re not always obvious.
Why Medicine Labels Don’t Tell You Everything
In the U.S., food labels are tightly controlled. The Food Allergen Labeling and Consumer Protection Act (FALCPA) and its 2023 update, the FASTER Act, force manufacturers to clearly list the nine major allergens: milk, eggs, fish, shellfish, tree nuts, peanuts, wheat, soy, and sesame. If a product contains any of them-even in tiny amounts-it has to say so. Either right in the ingredient list (like "lecithin (soy)") or in a "Contains:" line at the bottom.But none of that applies to pills, creams, or injections. The FDA doesn’t require drugmakers to list allergens in the same way. That means a capsule could contain lactose (a milk derivative), peanut oil, or soy lecithin-and you’d never know unless you dig deeper. In fact, a 2023 study in the Journal of Allergy and Clinical Immunology found that 4% of American adults have a documented allergy to at least one inactive ingredient in medication. Many of those reactions happen because the label doesn’t warn you.
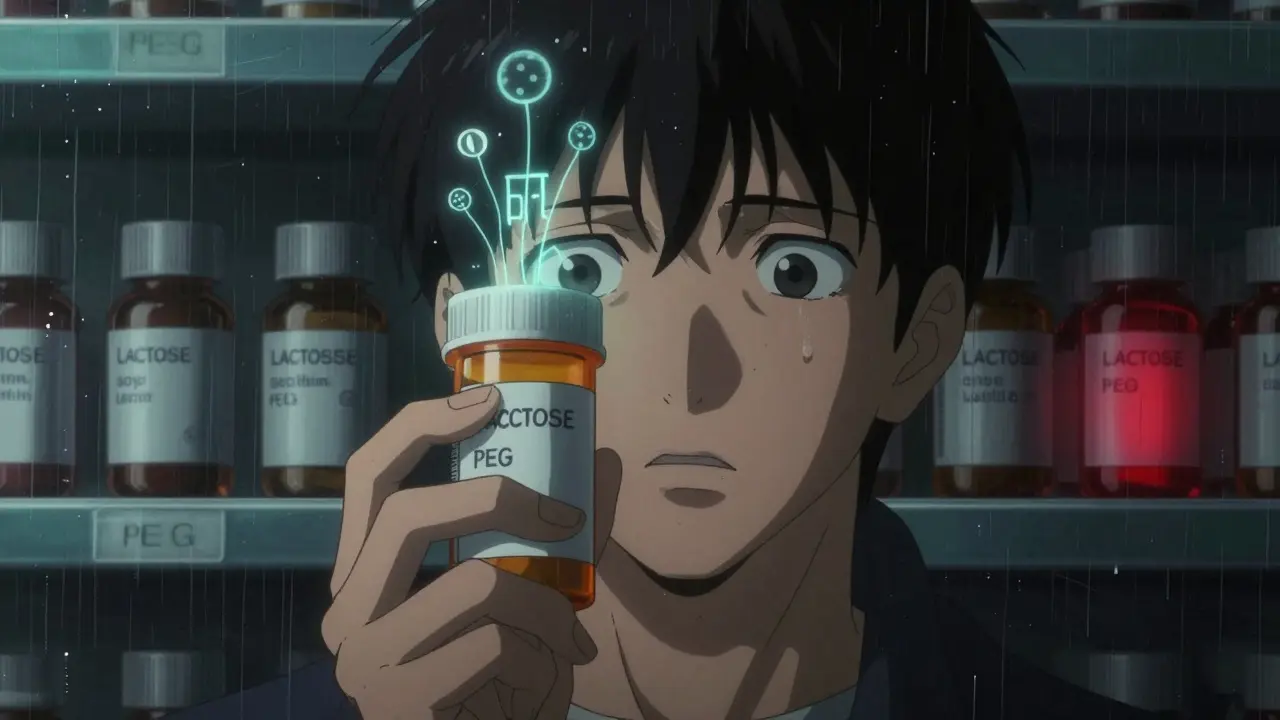
What Are Inactive Ingredients? (And Why They Matter)
Inactive ingredients are the fillers, binders, and coatings that help make a pill hold its shape, dissolve properly, or taste better. They’re not the active drug, but they can still trigger serious reactions. Common ones include:- Lactose - derived from milk. A problem for people with dairy allergies.
- Starch - often from corn or wheat. Can trigger gluten-sensitive individuals.
- PEG (polyethylene glycol) - found in many laxatives and vaccines. Linked to allergic reactions in some people.
- Artificial colors - like FD&C Yellow No. 5 (tartrazine), which can cause reactions in sensitive individuals.
- Peanut oil - used in some injectables. Even trace amounts can be dangerous.
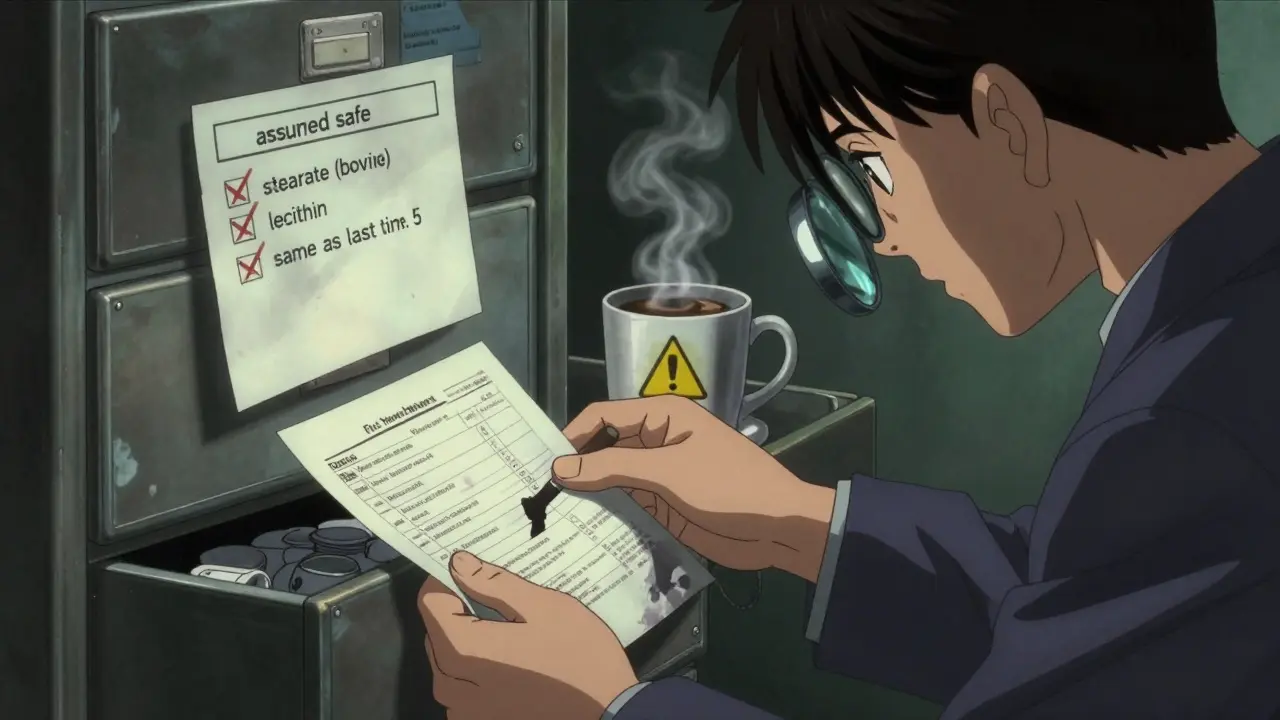
- Soy lecithin - used as an emulsifier. Often listed as "lecithin" without clarification.
These aren’t rare. A 2022 FDA report showed that nearly 1 in 5 generic medications contain at least one of these allergenic ingredients. And here’s the kicker: two different brands of the same generic drug can have completely different inactive ingredients. So if you’ve been taking Brand A for years and your pharmacist switches you to Brand B? You might be walking into a hidden risk.
How to Find Out What’s Really in Your Medicine
You can’t rely on the front of the bottle. The solution? Ask for the full list of inactive ingredients. Here’s how:- Ask your pharmacist - specifically request the complete list of inactive ingredients for your prescription. Pharmacists have access to detailed drug monographs and can print it out for you.
- Check the package insert - that small booklet inside the box often has a section called "Inactive Ingredients" or "Excipients." Look for it.
- Use the FDA’s DailyMed database - go to dailymed.nlm.nih.gov (no need to click, just know it exists). Search your drug name. Click on the "Label" tab. Scroll to the bottom of the "Description" section. That’s where inactive ingredients are listed.
- Keep a personal list - write down every medication you take and its inactive ingredients. Update it every time you refill. Include the manufacturer’s name too, since different makers use different fillers.
Don’t assume "generic" means "same." A 2023 Consumer Med Safety review found that 37% of people who had an allergic reaction to a medication did so after switching to a different generic version. The active ingredient stayed the same. The filler didn’t.
What to Do If You’ve Had a Reaction
If you’ve ever had a rash, swelling, or breathing trouble after taking a pill, even once, don’t brush it off. That’s not "just a coincidence." It could be an allergic reaction to an inactive ingredient. Here’s what to do:- Stop taking the medication - and call your doctor immediately.
- Get tested - an allergist can run skin or blood tests to identify specific sensitivities to ingredients like lactose, soy, or PEG.
- Ask for an alternative - many drugs come in formulations without common allergens. For example, some liquid versions of medications use alcohol or glycerin instead of lactose.
- Update your medical records - make sure your primary care doctor, pharmacist, and emergency contacts know your specific medication allergies.
Red Flags on Labels to Watch For
Some terms on medicine labels are vague and dangerous if you’re allergic. Here’s what to look out for:- "Lecithin" - could be soy, sunflower, or egg. If it doesn’t say which, ask.
- "Natural flavors" - not regulated. Could contain milk, wheat, or shellfish derivatives.
- "Stearate" - often derived from beef or pork fat. Not always disclosed.
- "Color added" - if it doesn’t specify the dye, it could be one linked to allergies.
- "Contains:" statements - these are rare on medicine labels. If you see one, treat it as a red flag. It’s unusual and might mean the manufacturer is being extra cautious.
And never assume "sugar-free" means "allergen-free." Many sugar-free pills use lactose as a filler. The word "sugar" on a label doesn’t mean the same thing as "lactose."
What About International Medications?
If you buy medicine overseas-or order online from another country-your protections vanish. Labeling rules vary wildly. A pill sold in Canada, the UK, or Australia might contain the same active ingredient as your U.S. version, but use different fillers. One patient in Hobart reported a severe reaction after buying a generic painkiller from a Thai pharmacy. The label listed "starch" but didn’t say it was wheat starch. She didn’t know until her doctor called the manufacturer.Stick to trusted pharmacies. If you’re traveling, bring enough medication with you. If you must refill abroad, have your doctor write a note with the exact name of the manufacturer and the inactive ingredients you need to avoid.
How to Stay Safe Long-Term
Building habits around medication safety takes time, but it’s worth it:- Always check the label - even if you’ve taken the drug for years. Manufacturers change fillers without warning.
- Use the same pharmacy - they’ll track your history and can flag changes.
- Carry a list - keep a small card in your wallet with your medication allergies and the names of the inactive ingredients you react to.
- Teach your family - if you live with others, make sure they know what to look for and what to do in an emergency.
- Use apps - tools like Medisafe or AllergyEats (launched in early 2024) now let you scan barcodes and cross-reference inactive ingredients with known allergens. They’re not perfect, but they help.
There’s no law forcing drugmakers to be as clear as food companies. But you don’t have to accept that. You have the right to know what’s in what you swallow. And with a few simple steps, you can protect yourself.
Do prescription labels have to list allergens like food labels do?
No. Unlike food, which must follow strict U.S. labeling laws under FALCPA and the FASTER Act, prescription medications are not required to list allergens in a standardized way. Inactive ingredients like lactose, soy lecithin, or peanut oil can be present without clear disclosure. You must ask your pharmacist for the full ingredient list.
Can generic drugs have different allergens than brand-name versions?
Yes. Generic drugs must contain the same active ingredient as the brand-name version, but they can use different fillers, binders, and coatings. A generic version of a drug might contain lactose while the brand-name version uses cornstarch. Always check the inactive ingredients when switching brands or generics.
What should I do if I have a reaction to a medication?
Stop taking the medication immediately and contact your doctor. If you experience swelling, trouble breathing, or a rash, seek emergency care. Ask your doctor to refer you to an allergist for testing. Once identified, update your medical records and ask for alternative formulations without the allergen.
Are "natural flavors" safe for people with allergies?
No. "Natural flavors" is a vague term that can include milk, soy, wheat, or even shellfish derivatives. The FDA allows this term without disclosure. If you have food allergies, always ask for a full ingredient breakdown from the manufacturer or pharmacist.
How can I find the inactive ingredients for my prescription?
Ask your pharmacist for the complete list. You can also search for your drug on the FDA’s DailyMed website (dailymed.nlm.nih.gov). Look under the "Description" section of the label. The inactive ingredients are listed there in detail. Keep a personal record and update it every time you refill.
Sarah Barrett
February 16, 2026 AT 03:48Mike Hammer
February 18, 2026 AT 03:13Betty Kirby
February 19, 2026 AT 11:19Kapil Verma
February 20, 2026 AT 18:36Mandeep Singh
February 21, 2026 AT 03:22Charlotte Dacre
February 22, 2026 AT 18:27Kaye Alcaraz
February 24, 2026 AT 12:57Josiah Demara
February 25, 2026 AT 10:27Daniel Dover
February 26, 2026 AT 12:01Esha Pathak
February 28, 2026 AT 06:21Erica Banatao Darilag
March 1, 2026 AT 21:40Chiruvella Pardha Krishna
March 2, 2026 AT 01:04