Missing a dose of your child’s medication can feel like a crisis. Your heart races. You panic. Did you just ruin their treatment? Should you give two doses now to make up for it? The truth is, most of the time, missing a dose isn’t a disaster-but how you respond makes all the difference. Giving the wrong response can be far more dangerous than the missed dose itself.
Why Doubling Doses Is Never the Answer
The most common mistake parents make? Giving a double dose to "catch up." It’s understandable. You want your child to stay on schedule. But children’s bodies don’t process medicine like adults’. Their livers and kidneys are still developing. A double dose can overwhelm their system, leading to drowsiness, breathing problems, seizures, or even organ damage. Dr. Sarah Verbiest’s 2023 review found that doubling doses in children under 12 increases the risk of severe adverse reactions by 278%. That’s not a small risk. That’s a life-threatening one. This is especially true for high-risk medications like opioids, seizure drugs, or chemotherapy agents. Even one extra milligram of morphine can cause respiratory depression in a small child. Never, ever double a dose.Time-Based Rules: What to Do Based on Dosing Frequency
The right action depends on how often your child takes the medicine. Most hospitals use clear time thresholds based on the dosing schedule. Here’s what works:- Once-daily meds: If you remember within 12 hours of the missed time, give it. If it’s been more than 12 hours, skip it. Don’t give it the next day early. Just go back to the normal schedule.
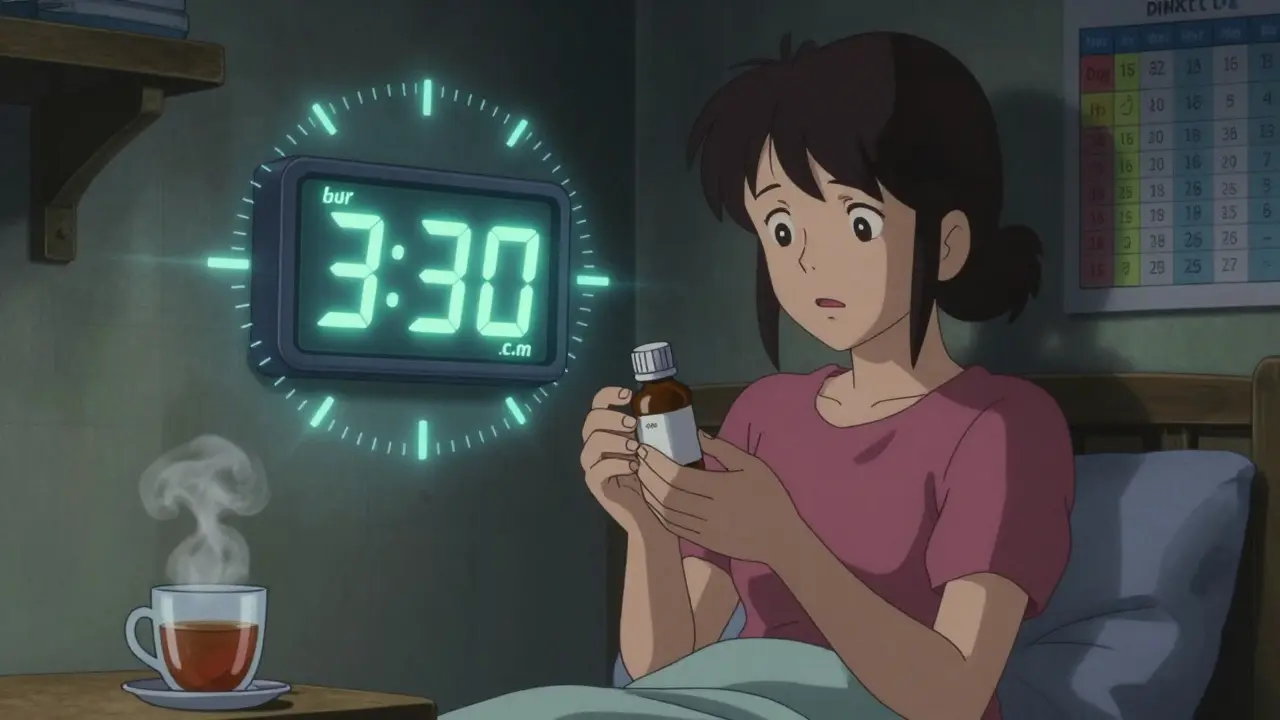
- Twice-daily meds (every 12 hours): If you miss a dose and remember within 6 hours, give it. After 6 hours, skip it. For example, if the dose is at 8 a.m. and 8 p.m., and you remember at 2:30 p.m., give it. If you remember at 3:30 p.m., skip it and wait until 8 p.m.
- Three times daily (every 8 hours): Give the missed dose if you remember within 3 hours. After that, skip it. If the doses are at 7 a.m., 3 p.m., and 11 p.m., and you miss the 3 p.m. dose but remember at 5:30 p.m., give it. If you remember at 6:15 p.m., skip it.
- Four times daily (every 6 hours): Give the missed dose if you remember within 2 hours. After that, skip it.
- Every 2-4 hours (as needed): If you miss a dose by more than 2 hours, skip it. Never stack these doses. This includes pain relievers or anti-seizure meds given on an as-needed basis.
When to Call the Doctor Immediately
Some medications are so critical that missing even one dose can affect treatment. These include:- Chemotherapy drugs
- Immunosuppressants (like for organ transplants)
- Anti-seizure medications (especially for children with epilepsy)
- Insulin or other diabetes medications
- Heart medications like digoxin
Why Instructions on the Bottle Are Often Not Enough
You’d think the label would tell you exactly what to do. But it often doesn’t. A 2021 review by the National Patient Safety Agency found that 25% of high-risk pediatric medications had no missed-dose instructions in their patient leaflets. That’s one in four. Many labels just say, “Take as soon as you remember.” That’s vague. Does that mean 1 hour? 6 hours? 12? Parents on forums like MedHelp and Reddit report confusion-especially when different medications give conflicting advice. One antibiotic says "take if remembered within 12 hours," while the seizure drug says "skip if more than 3 hours late." No wonder caregivers feel lost. That’s why you need to ask your provider for written instructions specific to your child’s regimen. Don’t rely on the bottle. Write down the rules for each medicine in a notebook or phone note. Include the time thresholds.
How to Avoid Missed Doses in the First Place
Prevention is always better than correction. Here’s what works:- Use a medication app: The American Academy of Pediatrics launched a free Pediatric Medication Safety Calculator app in 2023. It asks for the medicine, frequency, and time missed, then tells you exactly what to do. Beta users saw an 83% improvement in correct decisions.
- Set phone alarms: Label them clearly: "Emma - Amoxicillin - 8 a.m." Don’t just say "meds."
- Use a dosing chart: Boston Children’s Hospital found that color-coded charts (green for morning, yellow for afternoon, red for night) reduced missed doses by 44% in children with complex needs.
- Use oral syringes, not spoons: The FDA says household spoons vary by up to 40% in volume. A 5 mL syringe is precise. Buy them at any pharmacy-they’re cheap.
- Teach-back method: After your pediatrician explains the schedule, ask your child to repeat it back (if age-appropriate) or have you repeat it. Cincinnati Children’s cut missed doses by 37% using this simple trick.
Special Cases: Liquid Medications and Weight-Based Dosing
Liquid meds are the most common source of dosing errors. Why? Because they’re measured by weight. A child who weighs 15 kg needs a different amount than one who weighs 20 kg. Studies show that 73.8% of morphine errors in emergency rooms come from guessing a child’s weight by age alone. That’s dangerous. Always use a scale. If you don’t have one at home, ask your clinic to weigh your child at every visit and update the prescription. Length-based resuscitation tapes (like the Broselow tape) are used in hospitals to estimate weight based on height. They’re more accurate than age-based formulas. Ask your doctor if they recommend one for home use. It’s a small tool that can prevent big mistakes.What to Do If You’re Still Unsure
If you’re confused, don’t guess. Don’t wait until morning. Call your pharmacist. They’re trained to handle this exact question. Most have 24/7 lines. Or call your pediatrician’s after-hours line. Many hospitals now offer secure messaging through patient portals-use it. If you’re in a rural area with limited access, the National Rural Health Association found that families there have 3.2 times more medication errors than urban families. That’s why having a written plan is even more critical. Print it. Put it on the fridge. Save it in your phone.
How Common Are These Mistakes?
Medication errors affect 11% of preventable adverse events in hospitalized children, and dosing errors make up over a third of them. One in four caregivers can’t correctly answer when to skip or give a missed dose for a twice-daily medication. That number jumps to 68% for three-times-daily regimens. Parents of children with complex medical needs-those on four or more medications-report 300% more errors than other parents. That’s not because they’re careless. It’s because the system isn’t designed for complexity. The good news? Hospitals using standardized protocols have cut severe harm from medication errors by 52% since 2018. You can do the same with simple steps: know the rules, use tools, ask questions.What’s Changing in 2026?
The FDA now requires pharmaceutical companies to include clear missed-dose instructions on all pediatric medication labels. That’s new. And it’s coming fast. By 2026, you should see more consistent language on bottles: "Skip if more than 6 hours late" instead of "Take as soon as remembered." AI-powered tools are also rolling out. The NIH’s PediMedAI project, now in pilot, sends alerts 30 minutes before a dose is due. Early results show a 68% drop in missed doses for kids with chronic conditions. Smart dispensers that lock until the next dose time are also becoming more affordable. They reduce missed doses by 68% in clinical trials. If your child is on multiple daily meds, ask your insurance if they cover one.Final Rule: When in Doubt, Skip It
The safest default is always: skip the missed dose if you’re unsure. Missing one dose rarely ruins treatment. Giving too much can hurt your child. Your goal isn’t perfect timing-it’s safe timing. Keep a log. Write down when doses are missed and why. Share it with your pediatrician at every visit. That way, they can spot patterns-like if your child keeps missing afternoon doses because you’re at work-and adjust the schedule. Medication safety isn’t about being perfect. It’s about being smart. And smart means knowing when to give, when to skip, and when to call for help.What should I do if I miss a dose of my child’s antibiotic?
If it’s a once-daily antibiotic and you remember within 12 hours, give it. If it’s been more than 12 hours, skip it. For twice-daily antibiotics, give it if you remember within 6 hours. After that, skip it. Never double the dose. If you’re unsure, call your pharmacist. Most antibiotics are designed to work even if one dose is missed, as long as you get back on schedule quickly.
Can I give the missed dose if my child is sleeping?
If your child is asleep and the missed dose is within the safe window (e.g., less than 6 hours late for a twice-daily med), gently wake them. Give the medicine, then let them go back to sleep. But if it’s been more than the safe window, don’t wake them. Just wait until the next scheduled dose. Waking a child for a missed dose isn’t worth the stress if it’s too late.
My child vomited after taking the medicine. Should I give another dose?
If your child vomited within 15-20 minutes of taking the dose, it’s likely the medicine didn’t get absorbed. Give another full dose. If it’s been more than 20-30 minutes, don’t give another. The medicine is probably already in their system. Giving more could cause overdose. Always check with your provider if you’re not sure.
Is it safe to give a missed dose if I’m not sure how much was given?
If you’re unsure whether the dose was given, assume it was not. But only give it if you’re within the safe time window. For example, if it’s a once-daily dose and you think you might have given it at 8 a.m., but you’re not sure, and it’s now 10 a.m., you can safely give it. If it’s now 1 p.m., skip it. Better to be safe than risk giving two doses accidentally.
Why do some medicines have no missed-dose instructions on the label?
Many older medications were approved before current safety standards. A 2021 review found 25% of high-risk pediatric meds had no missed-dose guidance on their packaging. This is changing-FDA now requires it-but you can’t rely on labels alone. Always ask your doctor or pharmacist for clear instructions tailored to your child’s medicine and schedule.
Jodi Harding
January 17, 2026 AT 20:07Aysha Siera
January 18, 2026 AT 16:15rachel bellet
January 19, 2026 AT 02:36Pat Dean
January 20, 2026 AT 17:59Nishant Sonuley
January 21, 2026 AT 15:01Emma #########
January 23, 2026 AT 09:48Andrew McLarren
January 23, 2026 AT 19:42Andrew Short
January 24, 2026 AT 13:57Chuck Dickson
January 26, 2026 AT 12:43Robert Cassidy
January 28, 2026 AT 07:42Naomi Keyes
January 30, 2026 AT 00:18Andrew Qu
January 31, 2026 AT 18:33Zoe Brooks
January 31, 2026 AT 22:30Kristin Dailey
February 2, 2026 AT 19:58