When you hear the name levonorgestrel, you probably think of that handy “morning‑after pill” you keep in a drawer just in case. But how does this hormone actually affect your ability to get pregnant later, and what happens if you’re already pregnant when you take it? This article breaks down the science, the safety guidelines, and the practical take‑aways you need to make an informed decision.
What is Levonorgestrel?
Levonorgestrel is a synthetic progestogen used in many forms of hormonal contraception, most notably in emergency contraceptive pills (ECPs). It mimics the natural hormone progesterone, binding to the same receptors in the body to temporarily halt or alter the reproductive process. First approved by the FDA in the early 1990s, it has become one of the most widely studied and used contraceptive agents worldwide.
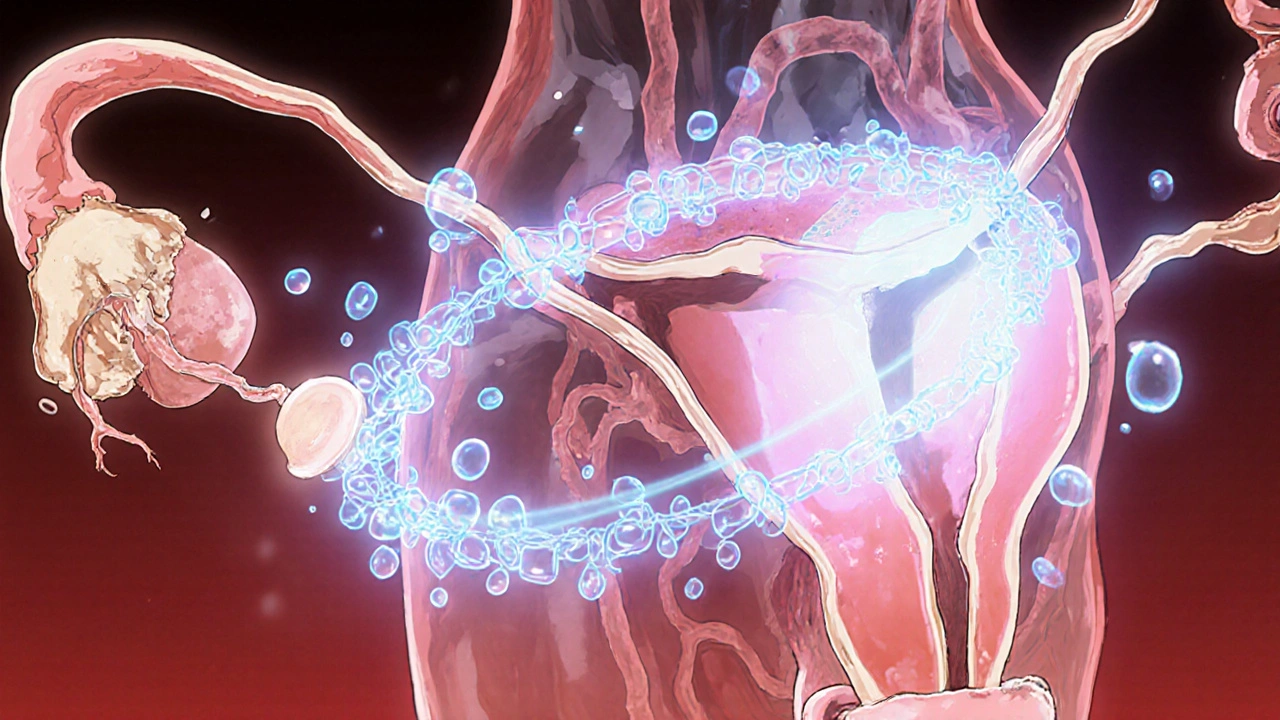
How Levonorgestrel Works
Levonorgestrel’s primary job is to prevent ovulation. By delivering a high dose shortly after unprotected sex, it disrupts the luteinizing hormone (LH) surge that would normally trigger the egg’s release. If ovulation has already occurred, the hormone thickens cervical mucus, making it harder for sperm to travel, and it can also alter the endometrial lining, creating a less hospitable environment for implantation.
Impact on Fertility - Short Term Effects
Most concerns revolve around whether a single dose can “damage” future fertility. The short answer: no. Clinical trials involving thousands of women have shown that a one‑time dose of levonorgestrel does not affect ovarian reserve, which is measured by anti‑Müllerian hormone (AMH) levels and antral follicle count. In other words, the pool of eggs you have is unchanged.
What does change briefly is the timing of your next period. Levonorgestrel can cause a delay of up to a week, simply because it meddles with the normal hormonal rhythm. Once the hormone clears from your system (its half‑life is about 24 hours), the menstrual cycle resumes its usual pattern.
Impact on Fertility - Long Term Effects
Long‑term data is reassuring. A 2022 meta‑analysis of 15 prospective studies followed women for up to five years after multiple uses of levonorgestrel‑based emergency pills. Researchers found no statistically significant difference in pregnancy rates, time to conception, or live‑birth outcomes compared with women who never used the drug. In short, using levonorgestrel repeatedly does not diminish your ability to become pregnant later.
What Happens If You’re Already Pregnant?
Levonorgestrel is intended to act before implantation. If you’re already pregnant-meaning a fertilized egg has implanted in the uterine lining-the hormone does not terminate an existing pregnancy. Large cohort studies from the United Kingdom and the United States, covering over 2 million pregnancies, have found no increased risk of miscarriage, congenital malformations, or adverse birth outcomes among women who inadvertently took levonorgestrel during the first trimester.
Nevertheless, because the drug can interfere with implantation, health agencies advise against taking it if you suspect you are already pregnant. The World Health Organization (WHO) classifies levonorgestrel as a Category 1 medication for emergency contraception-safe for most women-but it stresses confirming that pregnancy has not yet occurred before use.
Safety Profile and Regulatory Guidance
Levonorgestrel has a well‑documented safety record. Common side effects include nausea, fatigue, headache, and light spotting. These symptoms are usually mild and resolve within a couple of days. Serious adverse events, such as blood clots, are extremely rare and occur at rates comparable to those in the general population of non‑pregnant women.
The FDA permits over‑the‑counter sales of levonorgestrel ECPs to anyone aged 17 and older, with no prescription required. For younger teens, many states allow pharmacy‑based sales with parental consent. Internationally, the drug is listed on the WHO’s Model List of Essential Medicines, underscoring its global importance.
Comparing Emergency Contraception Options
While levonorgestrel is a solid choice, it isn’t the only game in town. Below is a quick comparison of the three most common emergency contraception methods.
| Method | Effective Window | Typical Failure Rate | Requires Prescription | Key Advantages |
|---|---|---|---|---|
| Levonorgestrel pill | Up to 72 hours | 0.6-2 % | No (OTC in many countries) | Readily available, inexpensive |
| Ulipristal acetate pill | Up to 120 hours | 0.5-1 % | Yes (prescription in most places) | Works later, maintains efficacy up to 5 days |
| Copper IUD | Within 5 days | <0.1 % | Yes (requires clinician insertion) | Provides ongoing contraception for up to 10 years |
Key Take‑aways for Real‑World Use
- One dose of levonorgestrel does not harm your long‑term fertility.
- The drug is safe for most women when taken within 72 hours after unprotected sex.
- If you’re already pregnant, levonorgestrel will not terminate the pregnancy but isn’t needed.
- Side effects are mild and short‑lived; serious complications are exceedingly rare.
- Consider other options like ulipristal acetate or a copper IUD if you need a longer window or higher efficacy.
Frequently Asked Questions
Can levonorgestrel cause long‑term infertility?
No. Multiple studies show that a single or even repeated doses do not affect ovarian reserve or future pregnancy rates.
Is it safe to take levonorgestrel while breastfeeding?
Yes. The amount transferred to breast milk is negligible, and the American Academy of Pediatrics considers it compatible with breastfeeding.
What if I vomit within two hours of taking the pill?
If vomiting occurs within two hours, repeat the dose with a new tablet and consider using a backup method until the next period.
Does levonorgestrel protect against sexually transmitted infections (STIs)?
No. It only prevents pregnancy. Use condoms or other barrier methods to reduce STI risk.
How does levonorgestrel differ from regular birth control pills?
Regular pills contain lower daily doses of estrogen and progestin to maintain a consistent cycle, while an emergency dose of levonorgestrel is much higher and intended for a single, short‑term intervention.
Understanding the science behind levonorgestrel helps you make smarter choices about emergency contraception without worrying about future fertility. If you have lingering doubts or a complex medical history, a quick chat with a healthcare provider can provide personalized guidance.
Doreen Collins
October 24, 2025 AT 17:45Hey there, just wanted to say that taking the morning‑after pill once isn’t going to ruin your future family plans. The hormone clears from your system in about a day, and your ovaries bounce back right away. Most women notice only a slight shift in their next period, which is totally normal. If you’re feeling anxious, give yourself a week and track your cycle – you’ll see everything’s back on track.
Kester Strahan
October 29, 2025 AT 10:45Yo, let’s break down the pharmaco‑kinetics real quick – levonorgestrel hits the LH surge like a blocker, preventing follicular rupture. If ovulation’s already in motion, the pill ramps up cervical mucus viscosity and tweaks the endometrium, making implantation less likely. The dosage is calibrated to hit a peak plasma conc. within 2‑3 hours, then the half‑life (~24 hrs) drops the level fast. This is why timing is key – the sooner you pop it, the higher the efficacy.
HILDA GONZALEZ SARAVIA
November 3, 2025 AT 04:45The data on levonorgestrel’s impact on long‑term fertility are actually quite reassuring.
The large prospective cohort studies involving tens of thousands of women have consistently shown no measurable change in ovarian reserve after a single emergency dose.
Anti‑Müllerian hormone levels, which are a reliable proxy for the quantity of remaining eggs, remain statistically unchanged when measured before and after use.
Similarly, antral follicle counts on ultrasound are identical, indicating that the drug does not deplete the follicular pool.
Short‑term cycle perturbations, such as a delayed or slightly heavier next period, are simply the result of a temporary hormonal reset.
Once the exogenous progestin is cleared, the hypothalamic‑pituitary‑ovarian axis re‑establishes its normal rhythm within one to two cycles.
Researchers have also looked at repeated use of levonorgestrel over several years, and the cumulative pregnancy rates remain comparable to control groups who never used emergency contraception.
A 2022 meta‑analysis of 15 studies with follow‑up periods up to five years reported no significant difference in time‑to‑conception or live‑birth outcomes.
Importantly, there is no evidence that levonorgestrel interferes with sperm quality or fertilization once ovulation occurs naturally.
The drug’s mechanism is primarily pre‑implantation; it does not affect an already implanted embryo, which is why miscarriage rates are not elevated in exposed pregnancies.
In the United Kingdom and United States databases covering over two million pregnancies, inadvertent first‑trimester exposure was not associated with increased congenital anomalies.
Side effects such as nausea, fatigue, or spotting are generally mild and resolve within a few days, and serious adverse events are exceedingly rare.
The World Health Organization classifies levonorgestrel as a Category 1 medication for emergency contraception, reflecting its safety profile when used correctly.
For women under 17, some jurisdictions require pharmacy oversight, but the overall accessibility has not compromised safety.
When comparing alternatives, ulipristal acetate offers a slightly higher efficacy window but requires a prescription, while a copper IUD provides the most effective emergency option yet is more invasive.
In everyday practice, levonorgestrel remains a cost‑effective, readily available choice that does not jeopardize future reproductive goals.
Amanda Vallery
November 7, 2025 AT 22:45Levono doesn’t mess up your future eggs.
Michelle Capes
November 12, 2025 AT 16:45I get why this can feel overwhelming 😊 – the key thing to remember is that the pill is meant to act before implantation, not after. If you think you might already be pregnant, a quick home test can give you peace of mind. Most studies show no increased risk of miscarriage or birth defects from an accidental dose. Take care of yourself and don’t hesitate to reach out to a healthcare provider if you have lingering concerns.
Dahmir Dennis
November 17, 2025 AT 10:45Well, isn’t it just adorable how we reduce complex reproductive biology to a handful of buzzwords and “quick fixes.” The reality is that any drug that meddles with your endocrine system deserves a thorough ethical debate, not a casual “pop it and move on” attitude. Levonorgestrel may block the LH surge, but it also exemplifies a broader societal trend of encouraging reckless sexual behavior under the guise of convenience. We’re celebrating a pill that lets people sidestep responsibility, while glossing over the importance of informed consent and comprehensive sexual education. If you truly care about reproductive health, demand more than a 24‑hour half‑life and a “fast‑acting” label – push for robust counseling and access to a full spectrum of contraceptive options.
Dawn Bengel
November 22, 2025 AT 04:45Honestly, all this “global health organization” talk is just a cover for pushing foreign pharma agendas on us 🇺🇸💊. Our own country has plenty of safe, home‑grown options; we don’t need to rely on a “one‑size‑fits‑all” pill that was marketed worldwide without proper American oversight. If you’re proud of being American, support home‑made solutions and question the imported hype. 👎
junior garcia
November 26, 2025 AT 22:45Picture this: you’re standing at a crossroads, a single pill in your hand, and the world seems to pause. That’s the power of levonorgestrel – a tiny burst of control in a chaotic moment. It’s not magic, but it’s the closest thing we have to a safety net.
Dason Avery
December 1, 2025 AT 16:45Exactly! Life hands us unexpected twists, and sometimes the best we can do is embrace the moment and trust the science to catch us when we fall 🌟. The emergency pill reminds us that we’re not powerless; we have tools, choices, and the audacity to keep moving forward. Keep shining, and remember that every setback is just a setup for a comeback 😊.
Casey Morris
December 6, 2025 AT 10:45Indeed, the pharmacodynamics of levonorgestrel, characterized by its rapid absorption, high bioavailability, and a half‑life of approximately twenty‑four hours, render it a quintessential example of modern contraceptive technology; yet, the discourse surrounding its societal implications remains regrettably superficial, often neglecting the nuanced interplay between endocrine modulation and psychosocial determinants of reproductive autonomy, which, if examined with due scholarly rigor, would illuminate the broader ethical canvas upon which such interventions are painted.
Teya Arisa
December 11, 2025 AT 04:45While the previous analysis offers an erudite perspective, it is essential to balance scientific scrutiny with empathetic guidance for those who may be navigating these choices for the first time. The evidence consistently indicates safety and efficacy, and healthcare providers should convey this with clarity and compassion. If you have questions, please consult a trusted medical professional. 😊
Marilyn Pientka
December 15, 2025 AT 22:45From a clinical pharmacology standpoint, levonorgestrel exerts its anti‑ovulatory effect via high‑affinity progesterone receptor agonism, thereby suppressing the pre‑ovulatory LH surge and augmenting cervical mucus viscosity; repeated administrations have demonstrated no statistically significant deviation in AMH trajectories, validating its non‑deleterious profile on ovarian reserve.
Lindy Hadebe
December 20, 2025 AT 16:45Sure, the data look solid, but at the end of the day it’s just another pill you can buy over the counter.