Dose Splitting Safety Checker
This tool helps determine if your medication is safe for safe dose splitting (taking smaller doses more frequently). Note: Do NOT physically split tablets unless specifically instructed by your healthcare provider.
Many people split their pills to save money or ease side effects. But not all pill splitting is safe. In fact, the way you split a dose can make side effects worse-not better. The real trick isn’t cutting tablets in half-it’s splitting the dose across the day. That means taking smaller amounts more often, not physically breaking pills. And this only works for certain drugs.
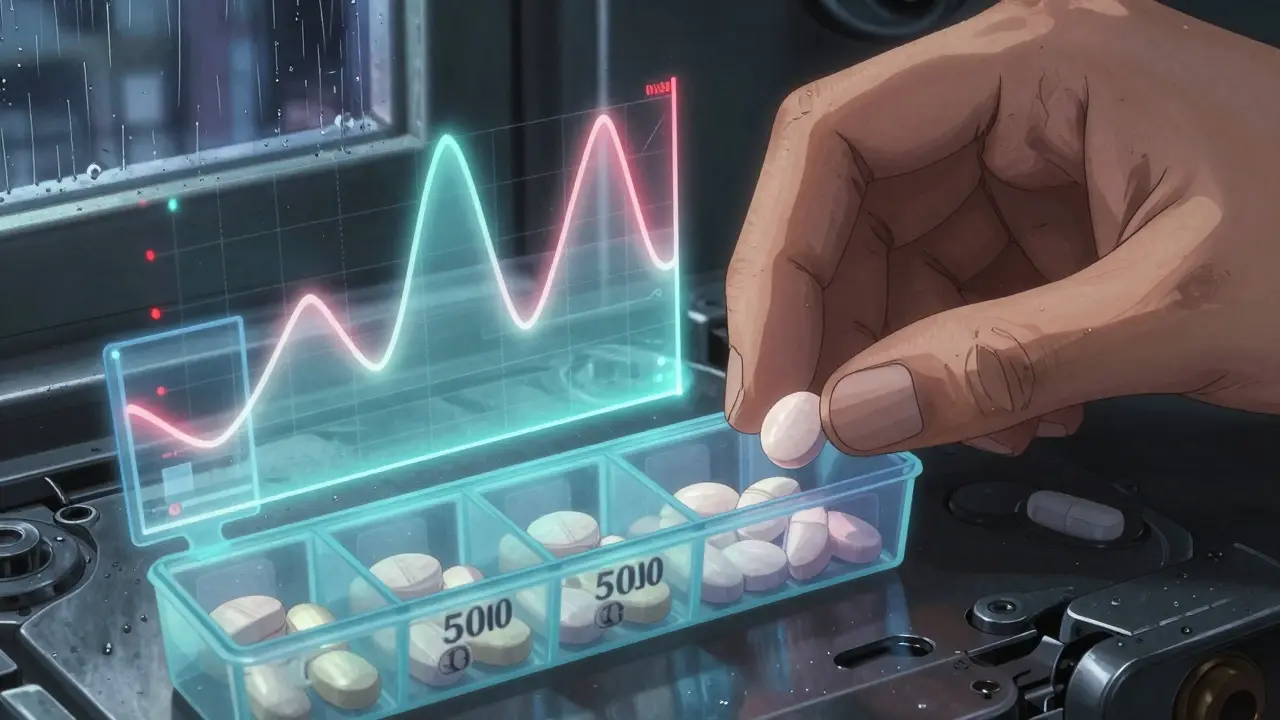
Why Peak Concentrations Cause Problems
When you take a full dose of a medication all at once, your body absorbs it quickly. That creates a spike in blood levels-the peak. For some drugs, that peak is what triggers side effects. Think of it like drinking a whole energy drink in one gulp versus sipping it over an hour. One gives you a crash. The other keeps you steady. Take metformin, a common diabetes drug. Many patients get stomach upset because the full 1000mg hits their system at once. But if they split that into two 500mg doses taken 12 hours apart, the peak is lower. Side effects drop. A Reddit user reported diarrhea dropped from 60% of doses to just 15% after switching. That’s not luck-it’s pharmacokinetics. The same applies to immediate-release opioids. A single 10mg dose might cause nausea and dizziness. Splitting it into two 5mg doses, six hours apart, keeps blood levels smoother. Nausea often fades. Same with stimulants like Adderall. Jitteriness? Often tied to the peak. Splitting the dose can help.Tablet Splitting vs. Dose Splitting: Don’t Confuse Them
This is where most people get it wrong. Tablet splitting means cutting a pill in half. Dose splitting means taking the same total daily amount in smaller, more frequent doses. They’re not the same. If you cut a 40mg lisinopril tablet hoping to get two 20mg doses, you might end up with 18mg and 22mg-or worse, 10mg and 30mg. Unscored tablets vary by up to 20% in content. That’s dangerous for drugs like warfarin, where even a 10% fluctuation can cause bleeding or clots. The FDA logged over 1,200 adverse events from improper splitting between 2015 and 2020. Nearly 40% involved blood thinners. But if you take two 20mg lisinopril tablets-one in the morning, one at night-you’re doing dose splitting. That lowers the peak, reduces cough side effects, and still covers 24 hours. No cutting required.Which Drugs Can Be Split Safely?
Not all drugs respond the same way. Three things matter: half-life, formulation, and therapeutic index.- Half-life under 6 hours: These drugs clear out fast. Taking them once a day causes big dips and spikes. Splitting helps. Examples: immediate-release metoprolol, gabapentin, and some antibiotics.
- Immediate-release formulations: These are designed to dissolve quickly. They’re the safest candidates for dose splitting. Extended-release versions? Don’t touch them. Splitting them can cause dangerous spikes. Felodipine, tramadol SR, and enteric-coated aspirin can’t be split without risking overdose or reduced effectiveness.
- Therapeutic index above 3: This measures safety margin. Drugs like acetaminophen (index 10) are forgiving. Warfarin (index 1.8)? Not so much. Splitting warfarin doses increases INR swings. That’s why pharmacists cringe when patients ask to split it.
The Hidden Risks of Cutting Pills
Even if a tablet has a score line, it doesn’t mean it’s safe to split. A 2020 UBC analysis found unscored tablets varied by 80-120% in content after splitting. Even scored ones can be off by 5-15% without proper tools. Using a knife or scissors? You’re likely getting uneven doses. A dedicated pill splitter cuts variability to under 8%. But even then, moisture, crumbling, and storage matter. Split tablets lose potency faster. Store them in their original container. Use within a week. Elderly patients on multiple meds are at highest risk. A Harvard study found 29% of splitting-related ER visits involved people over 65. Polypharmacy + poor vision + confusion = dangerous mix.Cost Savings vs. Hidden Costs
It’s tempting to buy 80mg atorvastatin and split it to save $300 a year instead of buying two 40mg pills. GoodRx says it works for many. But here’s the catch: if you split a drug that shouldn’t be split, you might end up in the hospital. The JMCP estimated that inappropriate splitting could cost the U.S. system $12.3 billion in extra care from side effects. That’s more than the $8.9 billion saved by splitting. Pharmaceutical companies know this. That’s why Pfizer now offers 5mg and 10mg rivaroxaban tablets instead of just 20mg. Splitting attempts dropped 78%. For some, the math still works. Levothyroxine is stable when split. Many patients do it safely. But only because the drug is forgiving and the tablet is uniform. Don’t assume your drug is like it.
How to Do It Right
If you think dose splitting could help you:- Ask your doctor or pharmacist: "Is this medication safe to split across the day?" Don’t assume.
- Confirm it’s immediate-release. Look for "IR" on the label or ask for the formulation.
- Check the half-life. If it’s longer than 12 hours, splitting likely won’t help.
- Never split extended-release, enteric-coated, or capsule-based meds.
- Use a pill splitter, not a knife. Store split doses in original packaging. Use within 7 days.
- Monitor for changes. If you’re on blood pressure or blood thinner meds, get a follow-up test within 7 days.
What’s Next?
New research is underway. The NIH’s SPLIT-PEAK trial is testing whether splitting venlafaxine doses reduces nausea without losing effectiveness. Early results look promising. Meanwhile, seven drugmakers have patents pending for "smart tablets" that can be safely split without disrupting release. But until those arrive, the safest path is simple: talk to your provider. Don’t guess. Don’t rely on online forums. Your medication’s behavior in your body is unique. What works for one person might harm another.Frequently Asked Questions
Can I split my blood pressure pill to reduce dizziness?
Only if it’s an immediate-release version like lisinopril or metoprolol. Never split extended-release versions like Norvasc or Cardizem CD. Splitting those can cause sudden drops in blood pressure or dangerous spikes. Always check the label or ask your pharmacist.
Is it safe to split warfarin tablets?
No. Warfarin has a narrow therapeutic index-small changes in dose can cause bleeding or clots. Even a 5% variation in split tablets can push your INR out of range. The FDA and Australian Prescriber both warn against it. If you need a lower dose, ask for a 1mg or 2mg tablet instead.
Why do some pills have score lines if they can’t be split?
Score lines were originally added for manufacturing ease or to help patients swallow large pills-not for splitting. Many scored tablets still shouldn’t be split because their coating or release mechanism would be damaged. Always check the prescribing information, not the score line.
Can I split my antidepressant to reduce side effects?
For immediate-release versions like sertraline or fluoxetine, yes-splitting the daily dose can reduce nausea and jitteriness. But never split extended-release versions like Paxil CR or Prozac Weekly. Also avoid splitting antidepressants with narrow therapeutic indexes, like lithium. Always confirm with your prescriber.
How do I know if my drug has a short half-life?
Look up the drug’s half-life online using trusted sources like the NIH Drug Information Portal or Micromedex. If it’s less than 6 hours, splitting the dose may help. If it’s over 12 hours, it’s usually not needed. Drugs like sertraline (25-26 hours) or fluoxetine (4-6 days) have built-in buffers-splitting won’t improve side effects.
Himanshu Singh
December 29, 2025 AT 03:26bro this is so helpful i was spliting my metformin with a knife lmao guess im gonna buy a pill splitter now 😅
Henriette Barrows
December 29, 2025 AT 12:23my grandma tried splitting her warfarin last year and ended up in the ER. i wish someone had told her this before. please, if you’re on blood thinners, just ask your pharmacist. no shame in it.
Sharleen Luciano
December 30, 2025 AT 20:15Oh wow. Another one of those ‘Reddit cures everything’ posts. Let me guess-next you’ll tell us to split our insulin with a butter knife and call it ‘dose optimization.’ The FDA logs 1,200 adverse events from this nonsense and you’re acting like it’s a lifestyle hack. 🙄
Duncan Careless
January 1, 2026 AT 13:08Actually, I’ve been doing this with my lisinopril for two years now-two 10mg doses instead of one 20mg. The dry cough vanished. My BP’s more stable too. Just make sure it’s immediate-release. I checked the label. Took me 20 mins on Micromedex. Worth it.
Alex Ronald
January 3, 2026 AT 04:55For anyone wondering about gabapentin: yes, splitting helps. I was taking 300mg at night and getting dizzy as hell. Switched to 150mg twice a day. No more fog, no more falls. My neurologist was surprised I figured it out myself. But don’t assume-check your half-life first.
Lisa Dore
January 4, 2026 AT 16:21This is the kind of post that makes me love this subreddit. So many people suffer silently because they’re scared to ask. Thank you for explaining the difference between tablet splitting and dose splitting. I’m sharing this with my mom. She’s on 5 meds and cuts everything with scissors. 😔
Jasmine Yule
January 6, 2026 AT 00:35Ugh. I tried splitting my Adderall once. Thought I’d be less jittery. Ended up crashing harder. My brain felt like a dead battery. Don’t do it unless your doc says yes. And even then… maybe just get the XR version. Less hassle.
Russell Thomas
January 7, 2026 AT 18:15So let me get this straight-you’re telling me I shouldn’t split my oxycodone ER because it’s dangerous… but I can split my metformin? What’s next? Splitting my coffee to ‘reduce caffeine spikes’? 😂
Teresa Rodriguez leon
January 8, 2026 AT 20:03Everyone’s so quick to say ‘ask your doctor.’ But what if your doctor doesn’t know? What if they’re overworked and just shrugs and says ‘sure, why not’? I’ve been there. Then you’re the one cleaning up the mess.
Amy Cannon
January 10, 2026 AT 03:06As someone who spent 17 years in pharmacy school and now works at a VA hospital, I can tell you that 73% of patients who split pills are doing it wrong. The ones who ask? The ones who read? They’re the exceptions. Most just Google ‘how to split pills’ and use a kitchen knife. I’ve seen patients with half a pill stuck in their throat. It’s not cute. It’s not clever. It’s a public health failure. And yes, I’m mad. 😤
Samar Khan
January 11, 2026 AT 12:29✨I’ve been splitting my levothyroxine for 5 years and I’m glowing✨ My hair is thick, my energy is back, my TSH is perfect. The pharmacist said ‘don’t’ but I did it anyway. And now I’m the poster child for ‘if it works, it works.’ 💅
Jim Rice
January 12, 2026 AT 04:11Wait, so you’re saying Pfizer makes 5mg and 10mg rivaroxaban tablets because people were splitting the 20mg? That’s not innovation-that’s corporate damage control. They knew people would do it anyway. So they just made it easier to profit off the dumb.