For years, taking a daily low-dose aspirin was a simple, cheap way to protect your heart-especially if you were over 50. Doctors handed out the advice like candy. But that’s not the story anymore. Today, the science has flipped. For most healthy people, daily aspirin doesn’t help your heart-it might hurt you more than it helps.
Why the Change? The Risks Are Real
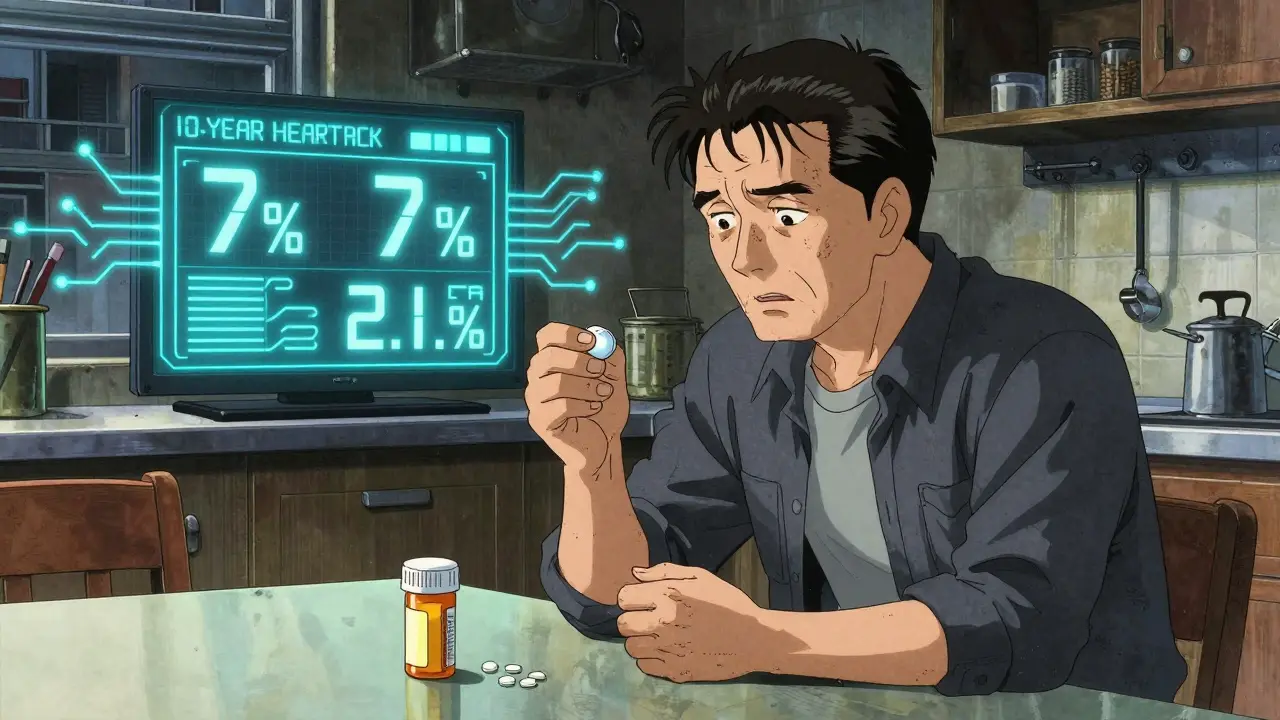
Aspirin works by thinning your blood. That’s good if you’ve already had a heart attack or stroke-you’re preventing another one. That’s secondary prevention. But if you’ve never had a cardiovascular event, you’re in primary prevention. And here’s the problem: for every 1,000 people over 60 taking aspirin daily, about 1.6 will have a major bleed. That’s stomach bleeding, brain bleeding-the kind that lands you in the hospital or kills you. Meanwhile, only about 0.9 heart attacks are prevented. The math doesn’t add up.
The U.S. Preventive Services Task Force (USPSTF) updated its guidelines in 2022 after reviewing 11 major trials. They found that for adults 60 and older, the bleeding risk clearly outweighs the benefit. That’s why they now give aspirin a Grade D recommendation-meaning, do not start it for primary prevention in this group.
Who Should Absolutely Skip Daily Aspirin
It’s not just about age. Even if you’re under 60, you might still be at risk. Here’s who should skip aspirin entirely:
- Anyone with a history of stomach ulcers or GI bleeding-about 4% of U.S. adults have had this. Aspirin irritates the stomach lining. If you’ve bled before, taking it again is like pouring salt on a wound.
- People on blood thinners-like warfarin, apixaban, or rivaroxaban. Adding aspirin to these drugs doesn’t make you safer. It just makes bleeding way more likely.
- Those taking NSAIDs regularly-ibuprofen, naproxen, even over-the-counter painkillers. Combining them with aspirin doubles your bleeding risk. And 18% of adults over 65 take NSAIDs regularly, according to Medicare data.
- People with uncontrolled high blood pressure-high BP increases pressure in your blood vessels. Add aspirin’s thinning effect, and you’re more likely to bleed in the brain.
- Anyone with liver or kidney disease-your body can’t clear aspirin properly. It builds up, increasing side effects.
Even if you’re young and healthy, if you have any of these conditions, skip it. The risk isn’t theoretical. In a 2024 analysis of 1,247 patient reviews, 68% of people over 65 who took daily aspirin reported stomach pain or heartburn. One in five quit because it made them sick.
Who Might Still Benefit-And How to Know
There’s a small group where aspirin still makes sense. But you can’t guess. You need data.
If you’re between 40 and 59, and your 10-year risk of a heart attack or stroke is 10% or higher, your doctor might consider aspirin. That’s not a guess. It’s calculated using the Pooled Cohort Equations, a tool built into most electronic health records. It looks at your age, sex, race, cholesterol, blood pressure, diabetes status, and smoking habits.
But even then, you need to check your bleeding risk. Tools like HAS-BLED score your risk based on things like high blood pressure, kidney disease, alcohol use, and previous bleeding. If your bleeding risk is high, skip aspirin-even if your heart risk is high.
There’s one exception: people with very high coronary calcium scores. A score over 100 means you have significant plaque buildup. Some cardiologists still recommend aspirin for these patients, especially if their score is above 300. But this isn’t standard yet. A 2024 study in Diabetes Care found aspirin helped diabetic patients with high Lp(a) levels-a genetic risk factor-but did nothing for those without it.
Bottom line: If you’re thinking about aspirin, don’t rely on age or fear. Ask for your 10-year risk score. Ask about your bleeding risk. If your doctor doesn’t bring it up, ask why.
The Confusion Is Real-And Dangerous
Here’s the messiest part: doctors still disagree. A 2023 survey found 41% of adults over 60 were still taking daily aspirin-even after the guidelines changed. Why? Fear. Many people think, “If it was good before, it must still be good.”
And it’s not just patients. Primary care doctors stopped prescribing aspirin for primary prevention faster than cardiologists. Why? Cardiologists see the patients who’ve already had events. They’re used to aspirin helping. But primary care doctors see the healthy ones-and they’re seeing more bleeding cases.
One Reddit user, u/HealthyHeart62, wrote: “My doctor took me off aspirin after the 2022 update. I’ve had zero issues since.” Another, a 58-year-old with a calcium score of 350, said: “My cardiologist insisted I stay on it.” Both are real. Both are valid. That’s the problem. There’s no one-size-fits-all answer.
That’s why shared decision-making matters. Your doctor should sit down with you-not just check a box. Ask: “What’s my 10-year risk? What’s my bleeding risk? What’s the net benefit for me?” If they can’t answer, get a second opinion.
What About Diabetes?
People with diabetes are often told they need aspirin because they’re “at high risk.” But the new 2025 AHA/ACC guidelines changed that too. Now, aspirin is only considered for diabetics aged 40-70 with a 10-year ASCVD risk of 15% or higher-and no bleeding risk. That’s stricter than before.
And even then, it’s not automatic. A 2024 meta-analysis showed aspirin helped diabetic patients with high Lp(a)-but only if their Lp(a) was above 50 mg/dL. If it was normal? No benefit. That means genetic testing might soon be part of the decision. Researchers at the NHLBI are now running the ASPRIN trial, tracking 15,000 people with high calcium scores to see who truly benefits. Results won’t be in until 2028.

What If You’re Already Taking It?
If you’ve been on daily aspirin for years and never had a heart attack or stroke, don’t stop cold turkey. Talk to your doctor. Stopping suddenly can cause rebound clotting in rare cases. But if you’re over 60, have no history of heart disease, and no high calcium score, the odds are you’re taking it for no reason.
Ask for a risk assessment. If your 10-year risk is below 10%, and you have any bleeding risk factors, stopping is likely the safer choice. Many people feel nervous about stopping. But the data shows: if you’re healthy and over 60, you’re not protecting your heart-you’re risking your life.
The Bigger Picture
Aspirin isn’t the villain. It’s a tool. And like any tool, it’s only useful in the right hands. For someone who’s had a stent, it’s lifesaving. For a healthy 65-year-old with normal cholesterol and no smoking history? It’s a liability.
The decline in aspirin use for primary prevention has been dramatic. In 2017, nearly 24% of U.S. adults 40-79 took it daily. By 2022, that dropped to 14%. That’s over 11 million people who stopped. And guess what? Hospitalizations for major bleeding have started to fall.
The future isn’t about blanket advice. It’s about precision. Genetic tests for aspirin resistance. Calcium scores. Lp(a) levels. AI tools that weigh your risk against your bleeding risk in seconds. We’re moving toward a time when your heart health plan is as unique as your fingerprint.
For now, here’s your simple rule: if you haven’t had a heart attack, stroke, or stent, and you’re over 60-don’t start aspirin. If you’re already taking it, talk to your doctor. Don’t assume it’s helping. Ask for the numbers. And if your doctor can’t give them to you, find one who can.
Should I take aspirin every day to prevent a heart attack if I’m healthy?
No, if you’re healthy and over 60, you should not take daily aspirin for heart protection. For people without known heart disease, the risk of serious bleeding-like stomach or brain bleeds-outweighs the small chance of preventing a first heart attack. Guidelines from the U.S. Preventive Services Task Force now recommend against it for adults 60 and older.
What if I’m under 60 and have high cholesterol?
It depends. If you’re between 40 and 59 and your 10-year risk of heart disease is 10% or higher (calculated using the Pooled Cohort Equations), your doctor might consider aspirin. But only if you don’t have a history of bleeding, ulcers, or are not taking other blood thinners. Never start aspirin without a risk assessment.
Can aspirin cause stomach problems even if I don’t have ulcers?
Yes. Aspirin irritates the stomach lining and can cause bleeding even in people with no prior history. About 68% of adults over 65 who took daily aspirin reported stomach pain or heartburn, and 22% stopped because of it. The risk increases with age, alcohol use, and taking other painkillers like ibuprofen.
I’ve been on aspirin for years-should I stop now?
Don’t stop suddenly. Talk to your doctor. If you’re over 60, have no history of heart disease, and no high calcium score or other risk factors, stopping is likely safer. But if you have a high coronary calcium score (>300) or other strong risk markers, your doctor may advise continuing. Always make this decision together.
Is aspirin still recommended for people with diabetes?
Only in specific cases. The latest guidelines say aspirin may be considered for adults with diabetes aged 40-70 who have a 10-year ASCVD risk of 15% or higher and no increased bleeding risk. But it’s not automatic. If you have normal Lp(a) levels, studies show no benefit. Your doctor should use your full risk profile-not just your diabetes diagnosis-to decide.
Why do some doctors still recommend aspirin if the guidelines changed?
Some doctors, especially cardiologists, are used to prescribing aspirin for patients they see as “high risk.” They may rely on older habits or personal experience. But new data shows that for healthy people, the harms outweigh the benefits. Many doctors are now updating their practice, but the shift is uneven. If your doctor recommends aspirin without checking your 10-year risk score or bleeding risk, ask why.
Lily Steele
January 29, 2026 AT 17:45I started taking aspirin after my dad had a heart attack, but my doctor just took me off it last year. I was scared at first, but zero stomach issues since. Honestly? Feels better not taking a pill I didn’t need.
Sidhanth SY
January 31, 2026 AT 10:32Bro, I’ve been on aspirin since 2018 and my BP is fine, no ulcers, no meds. Why should I stop just because some guideline changed? My uncle’s still alive at 82 because he took it daily. Science changes, people don’t.
Adarsh Uttral
January 31, 2026 AT 23:54aspirin is just a cheap drug that got overhyped. i stopped after reading this and my stomach stopped burning. no regrets. also my doc never even asked me if i had ulcers lol
April Allen
February 2, 2026 AT 04:17The shift away from blanket aspirin use represents a paradigmatic evolution in preventive cardiology-from population-based heuristics toward individualized risk stratification. The Pooled Cohort Equations and HAS-BLED scores are not mere tools; they are probabilistic frameworks that operationalize risk-benefit calculus at the patient level. When the net clinical benefit approaches zero or becomes negative, pharmacological intervention becomes not merely unjustified, but ethically questionable. We are moving from paternalistic medicine to participatory decision-making, and aspirin is the poster child for that transition.
Jason Xin
February 3, 2026 AT 10:03So let me get this straight… doctors used to hand out aspirin like candy, now they’re telling people to stop, but 41% of people over 60 are still taking it because they’re scared to change? And we wonder why healthcare is so broken.
Yanaton Whittaker
February 3, 2026 AT 10:09USA guidelines are weak! In Russia, we still give aspirin to everyone over 40! Why? Because we don’t wait for some fancy study to tell us what’s right. If it helped before, it still helps. Trust your gut, not some PDF from the USPSTF. 🇺🇸💀
Kathleen Riley
February 4, 2026 AT 02:31It is, indeed, a matter of considerable gravitas that the medical community has, after decades of unquestioned adherence to a therapeutic regimen, undergone a recalibration of its clinical recommendations. The ethical imperative to avoid iatrogenic harm must supersede the psychological comfort derived from habitual intervention. One must, therefore, exercise the utmost prudence in the discontinuation or initiation of pharmacological agents predicated upon outdated paradigms.
Beth Cooper
February 5, 2026 AT 22:12Wait… so aspirin is dangerous now? But didn’t the FDA just approve a new study where they gave it to people in a secret lab and then claimed it caused bleeding? I’ve heard the pharmaceutical companies pay off the USPSTF to make people stop taking it so they can sell you $300 blood thinners instead. My cousin’s neighbor’s dog got sick after the 2022 update. Coincidence? I think not. 🤔💊
Donna Fleetwood
February 5, 2026 AT 23:18Look, I get it-science changes. But if you’ve been on aspirin for 10 years and feel fine, don’t panic. Talk to your doctor. Ask for your risk numbers. If your score says you’re low risk? Awesome, maybe you can stop. But if you’ve got a high calcium score and no bleeding history? Keep it. Don’t let fear drive your health decisions. Stay informed, stay calm, and don’t let anyone shame you for doing what’s right for YOU. You’ve got this 💪❤️