SSRI Hyponatremia Risk Calculator
Assess Your Risk
Your Risk Assessment
Important: This tool assesses hyponatremia risk based on key factors identified in medical research. Always consult your healthcare provider for personalized advice.
Key Risk Factors Identified
Recommended Actions
Every year, hundreds of thousands of older adults in the U.S. start taking SSRIs for depression or anxiety. These medications help many feel better - but they also carry a quiet, dangerous risk: hyponatremia. And that risk doesn’t just stop at low sodium. It can lead to dizziness, confusion, falls, fractures, and even death. For people over 65, this isn’t a theoretical concern. It’s a real, preventable crisis hiding in plain sight.
What Is Hyponatremia - And Why Does It Matter for Older Adults?
Hyponatremia means your blood sodium level is too low - below 135 mmol/L. Sodium helps control fluid balance in your body. When it drops, water moves into cells, making them swell. In the brain, that swelling causes trouble: confusion, nausea, headaches, and muscle weakness. For older adults, these symptoms often look like normal aging. That’s why they’re missed. The real danger? Hyponatremia makes falls far more likely. Gait instability, dizziness, and weakness - all common signs of low sodium - are also top reasons older adults end up in the ER after a fall. A hip fracture at 75 isn’t just a broken bone. It’s often the start of a downward spiral: loss of independence, long-term care, even death. SSRIs trigger this by causing SIADH - syndrome of inappropriate antidiuretic hormone secretion. Normally, your body adjusts how much water it keeps based on need. SSRIs mess with that. Your kidneys hold onto too much water, diluting the sodium in your blood. It’s not about drinking too much. It’s about your body holding onto water when it shouldn’t.Who’s Most at Risk?
Not every older adult on an SSRI gets hyponatremia. But some are far more vulnerable:- Women - hormonal differences make them more sensitive to ADH changes.
- People with low BMI (under 25) - less body water means less buffer against dilution.
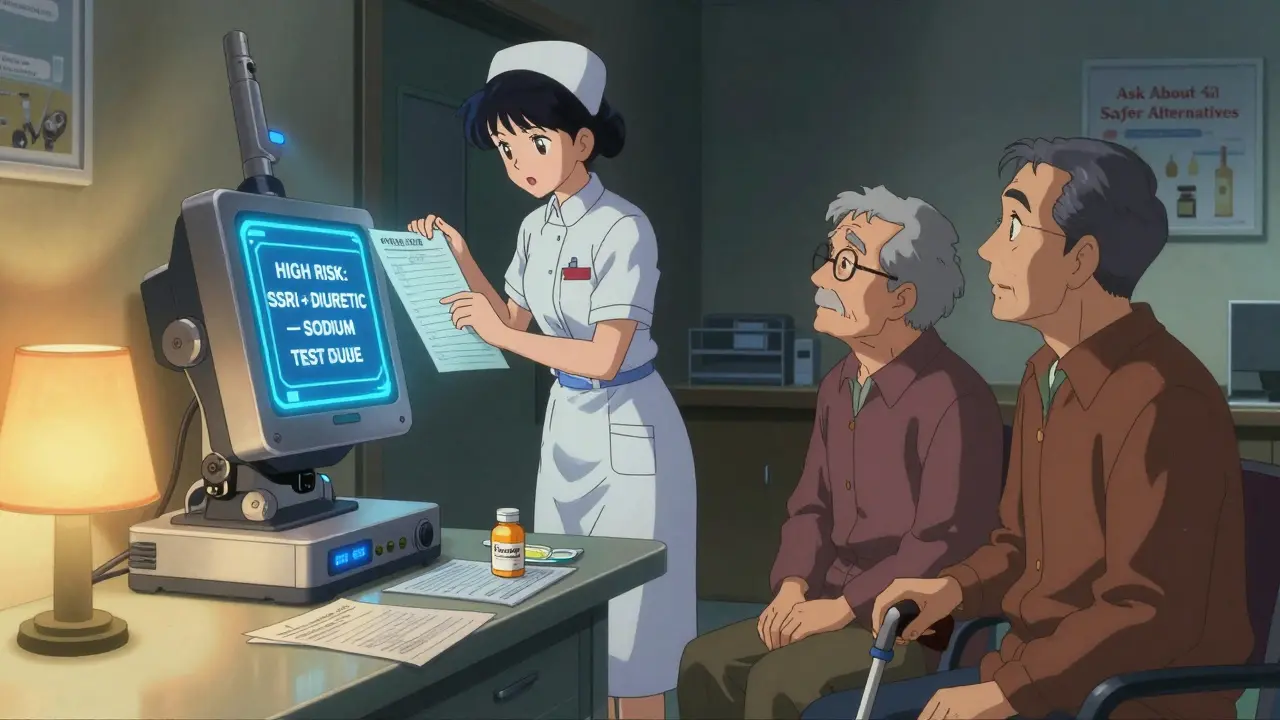
- Those on thiazide diuretics - this combo is a perfect storm. Thiazides flush out sodium, SSRIs trap water. Together, they raise hyponatremia risk by over 20%.
- People with sodium levels already near 140 - even a small drop can push them into danger.
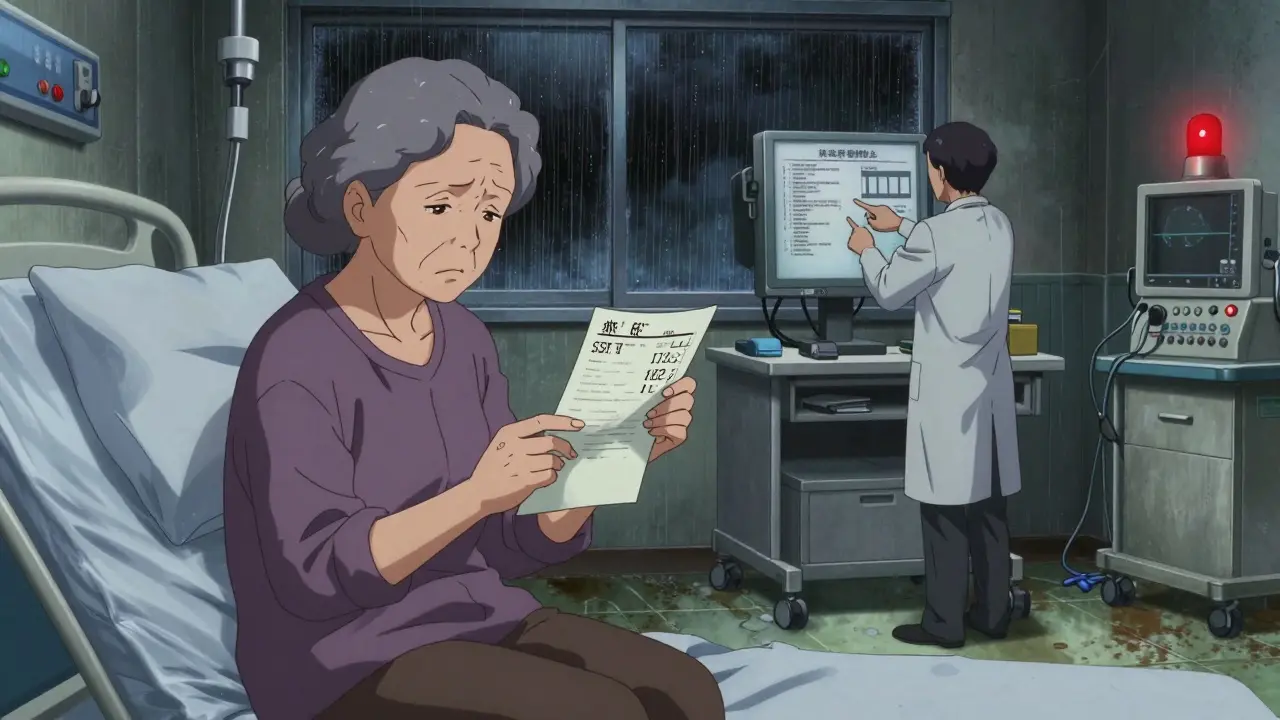
When Does It Happen?
Hyponatremia doesn’t creep in slowly. It usually shows up within two to four weeks after starting the SSRI - or after a dose increase. That’s why waiting for symptoms to appear is a dangerous gamble. Many people feel fine. They think the medication is working. But their sodium is dropping. Studies show 30-40% of cases are completely silent. No nausea. No headache. No confusion. Just a slow, silent decline in sodium. That’s why checking blood levels early isn’t optional - it’s lifesaving.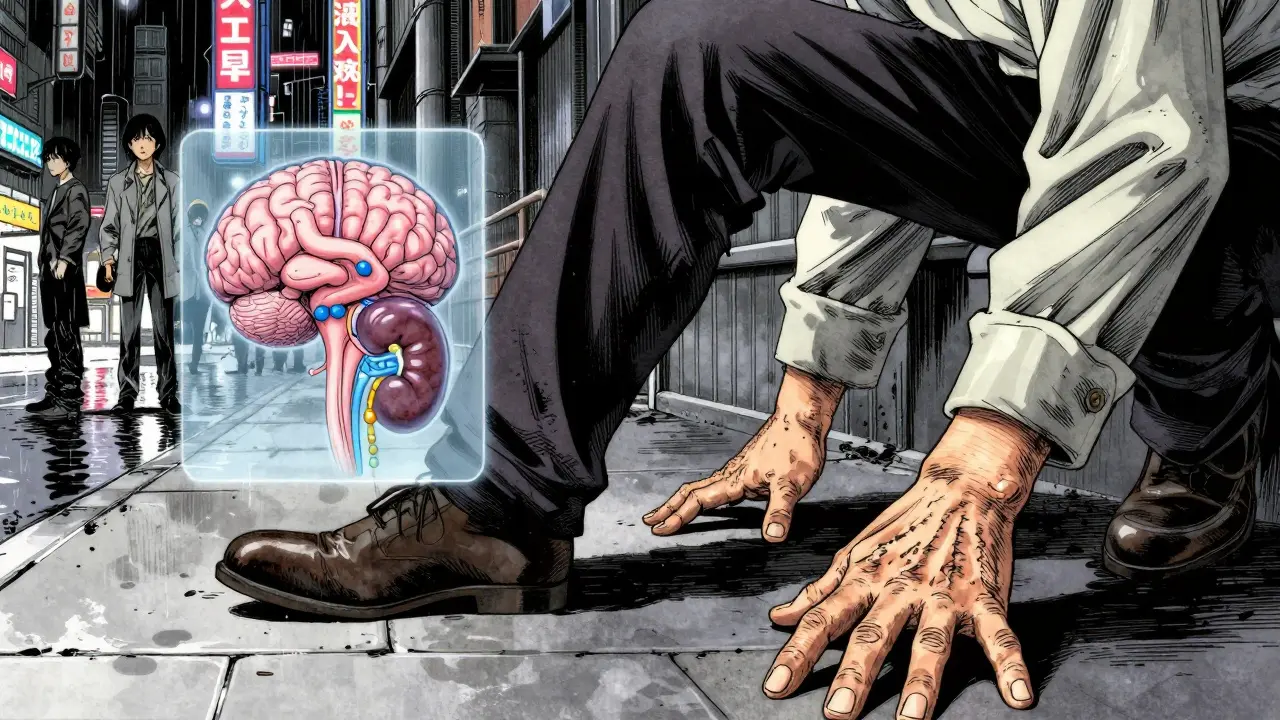
The Monitoring Debate: Do Tests Actually Help?
Here’s the contradiction: Every major guideline says to check sodium before starting an SSRI and again at two weeks. But a 2023 study in the Journal of the American Geriatrics Society found that doing these tests didn’t reduce hospitalizations. So why bother? The answer lies in what’s missing. Testing alone doesn’t help if no one acts on the results. A sodium level of 132 mmol/L might not trigger a hospital visit - but it should trigger a conversation. A dose change. A switch to a safer drug. A fall risk assessment. At Johns Hopkins Bayview Medical Center, clinics that followed a full protocol - baseline test, two-week follow-up, medication review, patient education - saw a 22% drop in hyponatremia-related ER visits. That’s not magic. That’s consistency. The problem? Many primary care offices don’t have systems to track these results. Nurses are overloaded. Doctors miss alerts. Lab results sit unread. That’s why AI tools are now being rolled out in 127 hospitals to flag high-risk combos like SSRI + thiazide and auto-schedule follow-up labs. It’s not perfect - but it’s better than hoping someone remembers.What Should You Do - If You or a Loved One Is on an SSRI?
If you’re over 65 and taking an SSRI, here’s what you need to do - right now:- Ask for a baseline sodium test before starting or restarting the medication. Don’t assume it was done.
- Request a repeat test at two weeks. Set a calendar reminder. Call the office if you don’t hear back.
- Review all your meds. Are you on a water pill? A diuretic? That’s a red flag. Ask your doctor if it’s still necessary.
- Know the warning signs: Unexplained dizziness, stumbling, confusion, nausea, or feeling weaker than usual. Don’t brush it off as ‘getting older’.
- Ask about alternatives. Is mirtazapine or bupropion an option? They work for depression and anxiety - and they don’t mess with sodium.
Preventing Falls Starts With Preventing Hyponatremia
There’s no direct study saying, “SSRI-induced hyponatremia causes X% more falls.” But the link is undeniable. Low sodium → dizziness → unsteady walking → fall → fracture → decline. The American Geriatrics Society updated its Beers Criteria in 2023 to list SSRIs as potentially inappropriate for older adults with existing hyponatremia or risk factors. That’s not a blanket warning - it’s a call for smarter choices. For someone with a history of falls, a low BMI, or on a diuretic, starting fluoxetine might be like lighting a fuse. Switching to mirtazapine could be the difference between staying independent and needing a walker. And it’s not just about pills. Therapy, exercise, social connection - these all help depression without touching sodium. But access is a barrier. Transportation, cost, stigma - they keep older adults from getting non-drug help.The Bigger Picture: Why This Is Getting Worse
SSRI prescriptions for Medicare beneficiaries rose 34% between 2015 and 2022. More people are being treated - that’s good. But more people are also at risk. Hyponatremia-related hospitalizations now cost over $1.2 billion a year in the U.S. alone. The FDA updated SSRI labels in 2022 to highlight this risk. But labels don’t change practice. Systems do. New tools are emerging: AI risk predictors that combine medication history, sodium levels, fall history, and age to flag who needs extra care. The NIH just funded a $2.8 million study to figure out the best monitoring strategy - because we still don’t know. Until then, the best defense is simple: know the risk. Test early. Ask questions. Push for safer options. And if you notice someone stumbling, confused, or unusually tired - don’t wait. Get their sodium checked.What If You’re a Caregiver?
You’re often the first to notice changes. If your parent or spouse on an SSRI starts:- Tripping more often
- Forgetting where they are
- Feeling nauseous without reason
- Appearing weaker or slower
Ryan van Leent
December 18, 2025 AT 22:11why do we even need to test sodium like its some kind of nuclear code its just a pill you take for feeling sad
jessica .
December 20, 2025 AT 08:23theyre putting ssris in the water supply dont you get it the government wants old people weak so they can control the nursing homes better
Sajith Shams
December 20, 2025 AT 14:22youre all missing the point. hyponatremia isnt caused by ssris its caused by the pharmaceutical industrys monopoly on endocrine regulation. the real culprit is the FDAs approval process which was designed by ex-merck executives. this is basic pharmacology 101.
Erica Vest
December 20, 2025 AT 16:05the data is clear: baseline sodium testing at initiation and repeat at 2 weeks reduces hospitalization risk by 22% in high-risk populations. this isnt speculation-its evidence-based geriatrics. if your clinic isnt doing this, theyre cutting corners. ask for it. insist on it. its not optional.
Chris Davidson
December 22, 2025 AT 03:08people these days are too lazy to read labels or take responsibility for their health. if you take a drug you should know the risks. its not the doctors fault you didnt ask. just stop complaining and get your blood work done
Dikshita Mehta
December 23, 2025 AT 04:02i live in india and we dont have routine sodium testing for ssris here but i’ve seen patients develop confusion and falls after starting fluoxetine. switching to mirtazapine helped dramatically. its not about fear-it’s about matching the drug to the person. simple really.
Chris Clark
December 24, 2025 AT 11:21my grandpa was on sertraline and started tripping over nothing. we asked for a blood test and his sodium was 131. doc switched him to bupropion and he’s been walking like a 40 year old again. dont ignore the little signs. theyre screaming.
William Liu
December 26, 2025 AT 03:40there’s hope here. we can fix this. we just need to listen to the science and stop treating depression like its a one-size-fits-all problem. safer meds exist. better systems exist. lets use them.
Aadil Munshi
December 26, 2025 AT 08:48ah yes the classic pharmaceutical cautionary tale. next youll tell me that aspirin causes stomach bleeds and sunlight causes skin cancer. everything has risks. the real tragedy is that we’ve turned medical care into a checklist ritual instead of a human conversation.
Frank Drewery
December 28, 2025 AT 03:52my mom was on fluoxetine and started forgetting her own name for a week. we thought it was dementia. turned out her sodium was 128. they stopped the med and she came back to us. dont wait for a fall. check the numbers.
Danielle Stewart
December 30, 2025 AT 02:11if you’re over 65 and on an SSRI, here’s your action plan: 1) call your doctor and ask for your last sodium level. 2) if you don’t have one, schedule a test. 3) ask if your diuretic is still necessary. 4) if you’re dizzy or stumbling, don’t wait. get checked. you deserve to stay strong.
mary lizardo
December 30, 2025 AT 12:07This article is a classic example of medical overreach disguised as concern. We have turned every minor physiological fluctuation into a crisis requiring intervention. The elderly are not fragile porcelain dolls. They are resilient. Let them live without being monitored like lab rats.
Kinnaird Lynsey
December 30, 2025 AT 21:44the irony is that the people most at risk are the ones least likely to speak up. if you’re a caregiver, your voice matters more than any guideline. if you see something, say something. gently. firmly. repeatedly. they might not thank you now-but they’ll thank you later.