You take a pill. It’s supposed to help. But you feel nothing. Or worse-you feel worse. You check the label. It’s not the brand you used to trust. It’s the generic version. Suddenly, the headache doesn’t fade. The anxiety creeps back. The muscle pain won’t quit. You didn’t switch because you wanted to. You switched because your insurance forced it. And now, you’re convinced the medicine doesn’t work anymore.
Here’s the truth: the pill in your hand is chemically identical to the brand-name version. Same active ingredient. Same dosage. Same absorption rate. The FDA requires generics to be within 80-125% of the brand’s performance. That’s not a loophole. That’s science. But your brain doesn’t care about bioequivalence. It cares about price, packaging, and perception.
Why a $0.02 Pill Feels Like It Does Nothing
In 2014, researchers at the University of Auckland ran a simple but startling experiment. They gave 87 college students with frequent headaches a placebo-no active drug at all. Half the pills were labeled with a well-known brand name. The other half were labeled as generic. Both groups got identical sugar tablets.
The brand-labeled placebo reduced pain by 2.3 points on a 10-point scale. The generic-labeled placebo? Only 1.1 points. That’s more than half the relief. And yet, both were nothing but starch and filler.
This isn’t magic. It’s psychology. Your brain has learned, over years of advertising and experience, that expensive things work better. That’s not irrational-it’s evolutionary. In the wild, high-cost resources usually meant higher quality. Your brain still thinks that way. So when you see a $0.02 generic pill next to a $4 brand-name one, your subconscious says: “This one’s cheaper. It must be weaker.”
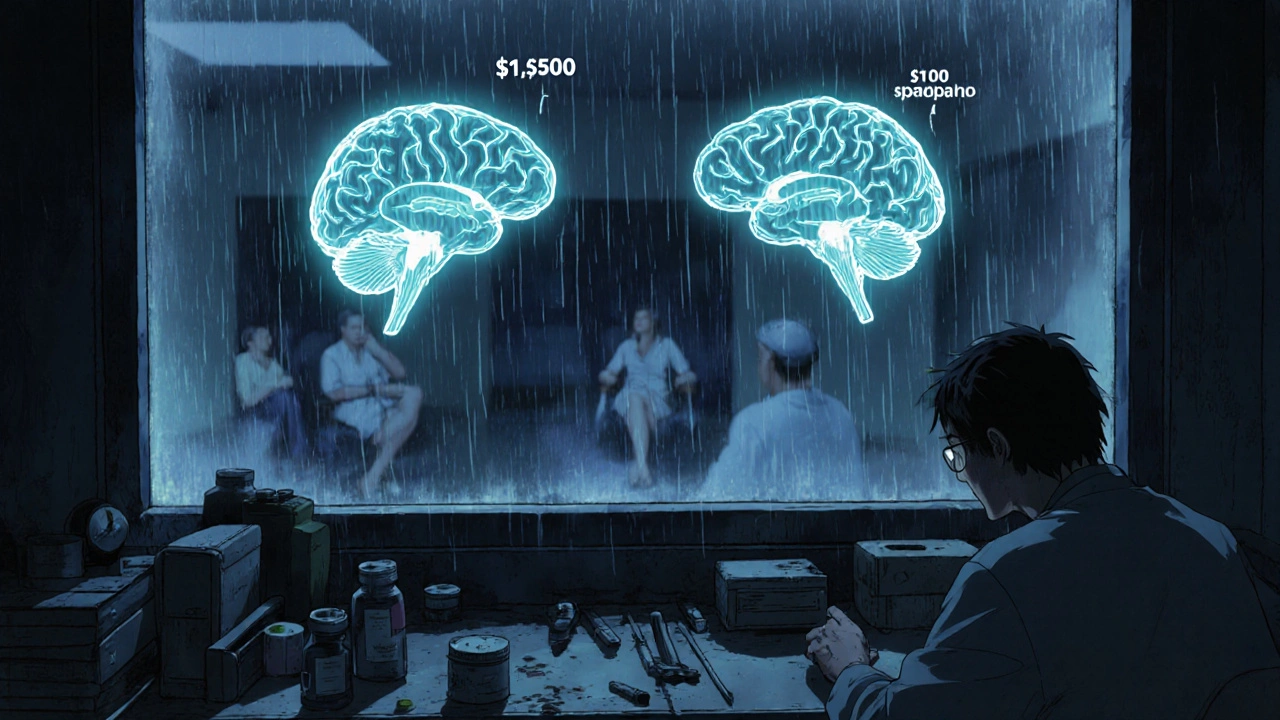
And it’s not just headaches. In a 2014 study from the University of Cincinnati, Parkinson’s patients got fake injections. One group was told it cost $1,500. The other, $100. The $1,500 placebo improved motor function by 28% more. Brain scans showed 53% more dopamine released in the group who thought they got the expensive treatment. Your expectations literally change your biology.
The Nocebo Effect: When Your Mind Makes You Sick
It’s not just that generics feel less effective. Sometimes, they make you feel worse. That’s the nocebo effect-the dark twin of the placebo effect. If you believe something will hurt you, your body finds a way to make it true.
A 2014 meta-analysis of 12 statin trials found that patients told they were taking a generic placebo reported more than twice as much muscle pain as those told they were taking the brand-name placebo. Same pill. Same dose. Same inactive ingredients. But the label changed everything.
On Reddit, people write: “Switched from Nexium to generic and my GERD came back.” “I got the generic antidepressant and now I’m dizzy all day.” “My seizures got worse after the pharmacy switched me.”
Doctors often assume these are real side effects. But when researchers monitor patients with EEGs, heart monitors, or blood tests, they find no biological difference. The symptoms are real-but they’re triggered by fear, not chemistry.
A 2021 survey by the Epilepsy Foundation found 39% of patients reported more seizures after switching to generics. Neurologists, reviewing their EEGs, concluded 78% of those cases were nocebo-driven. The brain, convinced the drug was inferior, triggered stress responses that lowered seizure thresholds.
Generics Are Cheaper. But Are They Really Worse?
Let’s cut through the noise. In 2023, 90% of all prescriptions in the U.S. were filled with generics. That’s 3.7 billion prescriptions. And the cost savings? $312 per patient, per year, on average. That’s not pocket change. That’s thousands of dollars for families. That’s millions for the system.
But here’s the catch: 18-24% of patients stop taking their generic meds within six months. Why? Because they believe they’re not working. Or worse-they believe they’re harming them.
That’s why hospitalization rates for patients on generics are 12-15% higher than for those on brand-name drugs. Not because generics are less effective. But because people stop taking them. Or take them inconsistently. Or panic when they feel a side effect that doesn’t actually exist.
And it’s not just about cost. It’s about control. When you’re handed a pill you didn’t choose, it feels like your doctor gave up on you. Like you’re being treated like a number. That feeling alone can trigger stress hormones that interfere with healing.
What Doctors Don’t Tell You (But Should)
Most doctors don’t have time to explain bioequivalence. A 15-minute appointment? They’re lucky if they get to the prescription before the next patient walks in.
But a 2018 study from the University of Chicago proved something simple: a seven-minute conversation changes everything. When doctors explained, “This generic version has the exact same active ingredient as the brand. It’s just cheaper. The FDA checks it just as closely,” patient acceptance jumped from 58% to 89%. Six months later, 72% of those patients were still taking their meds. In the group that got no explanation? Only 44% stayed on track.
There’s a technique called “positive generic messaging.” Instead of saying, “We’re switching you to generic,” say: “This is the same medicine, just more affordable. It works just as well, and it’s been tested on over 2,000 people to make sure.”
One doctor in Ohio started using this script. Within a year, his generic adherence rate went from 63% to 85%. His patients didn’t just take their pills-they thanked him.

What You Can Do Right Now
If you’ve been told to switch to a generic and you’re skeptical, here’s what to do:
- Ask your doctor: “Can you show me the bioequivalence data?” Most can pull up the FDA’s Orange Book on their tablet. You’ll see the exact numbers.
- Look up your drug on Drugs.com. Search for user reviews. You’ll find that 67% of people report no difference between brand and generic antidepressants. That number jumps to 82% when they’re told the truth about equivalence.
- Don’t assume your symptoms are from the pill. Ask: “Could this be stress? Could this be me expecting it to fail?”
- If you still feel off after a few weeks, talk to your pharmacist. Sometimes, switching to a different generic manufacturer helps. Not because the drug is better-but because the packaging, color, or shape feels more familiar.
There’s a study from the University of Wisconsin where researchers gave hypertension patients generic pills in fancy, branded-style packaging. The nocebo complaints dropped by 37%. It wasn’t the medicine. It was the look. The trust.
The Bigger Picture
This isn’t just about pills. It’s about how we value health. We’ve been sold the idea that expensive = better. That premium = safer. That if it’s cheap, it’s second-rate.
But medicine isn’t wine. It’s not a handbag. It’s science. And science doesn’t care about logos.
Yet our brains do. And that’s why we need to rewire how we think about generics-not by shaming people for their fears, but by giving them facts, respect, and control.
The $265 billion generic drug market isn’t just a cost-saving tool. It’s a public health lifeline. But if we don’t fix the psychology behind it, we’ll keep wasting billions on unnecessary brand prescriptions, higher hospital bills, and preventable suffering.
Next time you get a generic, don’t just swallow it. Think about it. Ask questions. Trust the science. And remember: the most powerful drug in your medicine cabinet isn’t the one in the bottle. It’s the belief that it will work.
Are generic drugs really the same as brand-name drugs?
Yes, by law. The FDA requires generics to contain the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also meet the same strict manufacturing standards. The only differences are in inactive ingredients (like fillers or dyes) and packaging. Bioequivalence testing ensures they work the same way in your body-within 80-125% of the brand’s performance. In over 98.5% of cases, there’s no meaningful clinical difference.
Why do I feel worse on generic medication?
It’s likely the nocebo effect. If you believe a generic is inferior, your brain can trigger real physical symptoms-headaches, dizziness, nausea, even increased pain or seizures-without any change in the drug’s chemistry. Studies show patients report more side effects from generics simply because they’re labeled as such. This isn’t in your head-it’s your brain’s response to expectation. Talking to your doctor about this can help reduce the effect.
Can the packaging of a generic drug affect how well it works?
Yes. A 2023 trial showed that when generic pills were packaged to look like brand-name drugs-similar colors, shapes, and labeling-patients reported 37% fewer side effects and higher satisfaction. Your brain uses visual cues to judge quality. If a pill looks familiar or premium, your body responds as if it’s more effective. This doesn’t change the drug’s chemistry, but it changes how your brain interprets it.
Is it safe to switch between different generic brands?
Yes, for most medications. The FDA allows multiple generic manufacturers, each with slightly different inactive ingredients. For drugs like blood pressure pills or antibiotics, switching between generics is safe and common. But for narrow-therapeutic-index drugs-like seizure meds or thyroid hormones-some patients report sensitivity to small changes. If you notice a difference after switching, tell your doctor. It may be nocebo, or it may mean you need to stick with one manufacturer.
Why do insurance companies push generics so hard?
Because generics cost 80-90% less than brand-name drugs. In 2023, generics made up 90% of prescriptions but only 23% of total drug spending. That saves the U.S. healthcare system billions each year. Insurance companies use generics to keep premiums lower for everyone. But if patients stop taking them because they believe they don’t work, those savings disappear-and costs rise again due to hospitalizations and complications.
Can learning about bioequivalence make generics work better?
Absolutely. A 2022 Drugs.com survey found that when patients were told generics are just as effective, 82% reported no difference between brand and generic antidepressants-up from 67% without that information. Knowledge reduces fear. When you understand the science, your brain stops expecting failure. That’s when the placebo effect works in your favor.
Tina Dinh
November 29, 2025 AT 20:40Andrew Keh
December 1, 2025 AT 12:39Sara Shumaker
December 1, 2025 AT 23:21Peter Lubem Ause
December 3, 2025 AT 13:57linda wood
December 4, 2025 AT 18:59gerardo beaudoin
December 6, 2025 AT 08:09Richard Thomas
December 6, 2025 AT 23:46jamie sigler
December 7, 2025 AT 17:51Bernie Terrien
December 9, 2025 AT 03:21Subhash Singh
December 10, 2025 AT 08:50Geoff Heredia
December 10, 2025 AT 12:19LINDA PUSPITASARI
December 12, 2025 AT 03:38